General objective: To develop a literature review that allows the analysis of risk factors and complications in preterm and low birth weight infants.
Method: The literature review took as a reference the Scielo database, which largely had articles published with thematic axes related to the topic under analysis, and other databases and journals that met the index of relationship with the topic under review were also taken. Although they were to a lesser extent, they were included in the review.
Result: In the review and analysis of the studies, it was found that prematurity and low birth weight increase vulnerability to various complications, mainly the immaturity of the organs and systems of the body is a key factor. The lungs, central nervous system, and other organs may not have fully developed, increasing the risk of breathing problems, infections, and difficulties in thermal regulation. Lack of time in the womb can also affect the development of the immune system, leaving them more susceptible to disease.
Conclusion: Preterm and low birth weight newborns face a number of challenges that require comprehensive, specialized care. Understanding these risk factors and complications is essential to providing the necessary care and improving the prospects of these little fighters from the beginning of their lives.
Keywords:
Preterm, Low weight, Complications, Risk factor, Physiology
Preterm and low birth weight newborns face a number of significant challenges that require specialized medical care and a comprehensive approach to ensure their proper health and development. This population of infants has unique characteristics that demand a deep understanding of their needs and careful management by health professionals.
First of all, it is crucial to highlight that premature babies are born before completing the normal gestation time, implying that their organs and systems have not had enough time to fully develop. This factor contributes to increased vulnerability to medical complications, as organs, such as the lungs and immune system, may not be fully mature.
Low birth weight, usually defined as weighing less than 2.5 kilograms, is another risk factor that may be associated with prematurity. These babies may have difficulty maintaining body temperature, face breathing problems, and be at increased risk of infections due to the immaturity of their immune system.
Intensive neonatal care becomes a crucial component for these newborns, as many of them require specialized care in neonatal intensive care units (NICUs). Constant monitoring, medication management, and specialized care are essential to address potential complications and ensure healthy development.
In addition to medical challenges, the situation of premature and low birth weight newborns also affects their families. Parents can experience significant levels of stress and anxiety, and the active involvement of parents in care and decision-making becomes critical to the baby's overall well-being.
Advances in neonatal medicine have greatly improved survival rates and quality of life for these babies, but challenges remain. It is crucial to not only address immediate medical needs, but also provide long-term support for the cognitive and emotional development of these children.
In this context, the situation of premature and low birth weight newborns is complex and requires comprehensive care that addresses both medical and emotional aspects. Collaboration between health professionals, family members, and communities is essential to ensure the best possible outcome for these babies in terms of health and development throughout their lives.
Theoretical-Conceptual Framework
Preterm newborns, also known as premature or preterm babies, are those born before completing 37 weeks of gestation, compared to a typical gestation period of around 40 weeks. These babies canes experience a number of challenges because they haven't had enough time in the womb to fully develop their organs and systems.1
Some important characteristics and considerations about preterm infants include:
Incomplete Development: Prematurity can affect the development of various organs and systems, such as the lungs, central nervous system, immune system, and others. This can make premature babies more prone to health problems and medical complications.
Low Birth Weight: Premature babies often have a birth weight lower than normal, usually less than 2.5 kilograms. Being underweight can be associated with a number of challenges, including difficulty maintaining body temperature, breathing problems, and an increased risk of infections. Neonatal Intensive Care Unit (NICU): Many premature newborns require specialized care in neonatal intensive care units. These units are equipped to provide intensive medical care, constant monitoring, and necessary support for premature infants.2
Medical Complications: Premature babies canes face a variety of medical complications, including breathing difficulties (respiratory distress syndrome), problems with feeding, risk of infections, and neurological problems. Treatment and specialized medical care are critical to addressing these complications. Long-Term Development: Although many premature babies outgrow initial complications, some may experience long-term challenges in terms of cognitive, motor, and emotional development. Long-term follow-up by healthcare professionals is essential to address any ongoing needs.3
Parental Involvement: Active parental involvement in care and decision-making is crucial to the well-being of premature infants. Parents are often trained to care for their children at home, and the formation of strong bonding is encouraged.
A neonatal medicine advances, significant advances have been made in the care of preterm infants, improving survival rates and quality of life. However, it remains an area of critical care that requires multidisciplinary approaches and personalized care for each premature baby.4
On the other hand, low birth weight newborns are those whose birth weight is less than 2.5 kilograms (5.5 pounds). This condition can occur regardless of the length of gestation, although it is more common in premature babies, born before 37 weeks gestation. Low birth weight can have a variety of causes and is associated with a number of medical and developmental considerations. An analysis of the situation of low birth weight infants takes into account the following points:5
Causes and Risk Factors: Low birth weight babies may result from prematurity, meaning they haven't had enough time to fully develop in the womb. Other causes may include intrauterine growth restriction (IUGR), in which the baby does not grow properly in the womb due to problems with the placenta or other conditions. Maternal factors such as malnutrition, smoking, drug use, and certain diseases can increase the risk of low birth weight.
Medical Complications: Babies with low birth weight are more likely to face medical complications, such as breathing problems, difficulty regulating body temperature, and increased risk of infections. Immaturity of organs, especially the lungs, can lead to conditions such as respiratory distress syndrome. Neonatal Intensive Care Unit (NICU): Many low birth weight newborns require specialized care in neonatal intensive care units for intensive care, constant monitoring, and nutritional support.6
Specialized Care and Nutrition: Low birth weight babies often require specific care and nutrition to promote proper growth and development. Breastfeeding can be more challenging, and some babies may need special formulas or nutritional supplements. Long-Term Development: Although many low birth weight babies outgrow initial complications, some may experience long-term challenges in terms of cognitive and motor development. Ongoing medical follow-up is essential to address any needs as the baby grows.
Family Support: The situation of having a baby with low birth weight can generate stress and anxiety in parents. Providing emotional support and education to families is crucial to help them cope with challenges.7
In that sense, low birth weight newborns require specialized care and a comprehensive approach that addresses both immediate medical needs and long-term aspects of their development. Collaboration between health professionals and families is critical to ensuring the well-being of these babies and facilitating their transition to a healthy life.8
To address the low birth weight preterm infant, nurses often apply a variety of theories and approaches that focus on providing specialized care and support to both the infant and his or her parents. A nursing theory relevant to this population is the NIDCAP (Newborn Individualized Developmental Care and Assessment Program) Theory of Developmental Care.9
This theory focuses on recognizing and attending to the individual needs of the premature infant, recognizing that each child is unique and responds differently to their environment and care. Here are some key elements of how this theory can be applied:
Individualization of Care: NIDCAP theory advocates individualization of care, recognizing the differences in the responses and needs of each premature infant. Nurses continually assess the baby's cues and responses to tailor care in a personalized way.
Reduced Environmental Stress: The neonatal intensive care unit (NICU) environment can be stressful for premature infants. Nurses work to reduce environmental stress, controlling lighting, noise, and stimulation to create a calmer environment conducive to development.
Fostering the Parent-Child Bond: Parents are encouraged to actively participate in the care of their premature infants. Nurses facilitate skin-to-skin interaction (kangaroo care) and support breastfeeding when possible. This contributes to the strengthening of the emotional bond between parents and baby. Emotional Support for Parents: Recognizing the stress and anxiety that parents may experience, NIDCAP theory also emphasizes emotional support for families. Nurse practitioners provide information, education, and resources to help parents understand and participate in their baby's care.10
Continuous Developmental Assessment: NIDCAP theory advocates the ongoing assessment of the development of the premature baby. Nurses observe the baby's responses to stimuli and adjust care as needed to support sensorineural development.
Promotion of Infant Autonomy: The autonomy of the premature infant within his or her abilities is promoted. This may include allowing the baby to participate in decision-making related to his or her care and respecting his or her developmental pace.
The application of NIDCAP theory or similar approaches in nursing care for low-birth weight preterm infants contributes to more developmentally focused and personalized care. Not only does this address immediate medical needs, but it also supports the premature baby's long-term growth and development. Collaboration between nurses, other members of the health care team, and parents is essential to the success of this approach.11
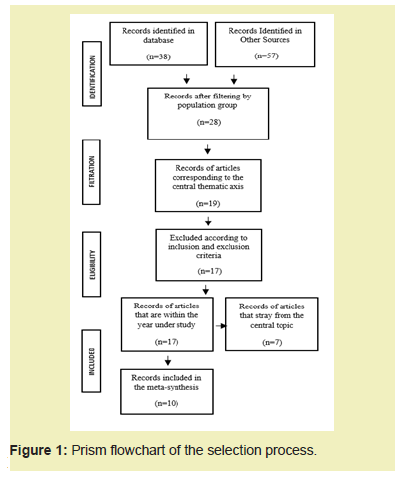
Scientific sources in the network were consulted for information, and the review was carried out in accordance with theoretical principles by collecting data from various databases, including Scielo, and other information databases, among others, without restricting any sources. The framework developed in the review covers a topical topic and studies that are currently being published.
Years in which a parameter has been published in the last three years have been taken into account for the inclusion criterion. (2019 to 2024). In response to the main objective, it also takes into account the remarkable contribution to the epistemological contribution. In addition, the essay complies with ethical presumptions in research and adheres to the latest edition of the American Psychological Association's guidelines for the publication of scientific texts Figure 1.
Risk Factors Associated with Early Neonatal Sepsis in Preterm Infants
The World Health Organization recommends a minimum of 6 prenatal check-ups to ensure a healthy pregnancy and prevent any type of complication, such as the detection of other risk factors for maternal perinatal morbidity. An insufficient number of prenatal clinics, defined as fewer than 6 check-ups, could jeopardize the course of pregnancy. This is another factor that has proven to be statistically significant. This finding aligns with that of the Mercedes de Paita Hospital, where it was identified that having fewer than six prenatal checkups was a risk factor for early neonatal sepsis. Fewer than six prenatal checkups were linked to early neonatal sepsis in a study that included 32 cases and 64 controls at Dos de Mayo National Hospital. By comparison, researchers at the Hospital de Iquitos found that pregnant women who had fewer than six prenatal checkups had a higher incidence of early neonatal sepsis than those who had six or more.12
Risk Factors Associated with Low Birth Weight
Acknowledging the intimate relationship between anemia and LBW, many authors also underscore the critical importance of preconception reproductive risk surveillance for the spouse to rapidly reduce or eliminate risks. Moreover, all non-pregnant women with possible risk factors for anemia between the ages of 15 and 49 should receive the nutritional supplement known as Mufer, which is manufactured in Cuba and contains iron and folic acid.
Premature rupture of membranes causes 38% of babies with low birth weight, mainly in boys, as indicated in the medical reference that was read. Premature rupture of membranes is facilitated by vaginal infection.
In their study, Vera et al. found that most pregnant women had a related disease, with vaginal infections, anemia during pregnancy, bronchial asthma and hypertension being the main causes of low birth weight.
In terms of gestational age at delivery, the results of this case study align with those of Montero et al., who found that mothers who gave birth before 37 weeks were 30 time more likely to experience a birth plan problem (PPN) and that preterm birth was a significant risk factor for PBN. One of the most important factors influencing the quality of life of a woman and her child throughout pregnancy is their nutritional status before and during. The main causes of delayed intrauterine growth are the mother's nutritional status, her energy intake, and her limited weight gain during pregnancy.
Low birth weight and preterm birth have been linked to anemia. Pregnancy-related anemia is the most common, and due to increased iron intake, 75% of all anemia diagnoses are directly related to iron deficiency. One of the most prevalent causes of low birth weight is chronic hypertension, which also has an impact on pregnancy outcome due to the medications needed to manage it. Preeclampsia in pregnancy, therefore, increases the chance of perinatal morbidity and death, which is linked to an increased frequency of fetal distress and delayed onset of intrauterine growth.
Risk Factors for the Development of Retinopathy of Prematurity
The "Technical Health Care Standard for Preterm Infants at Risk of Premature Retinopathy," published by the Peruvian Ministry of Health, is intended to prevent morbidity and blindness in premature infants and improve the overall health of the infant population. The main risk factors for COPD are considered to be gestational age < 37 weeks and weight < 2000 grams. According to the "Technical Reference Standard for the Control of Growth and Development of Children Under 5 Years of Age", a child's birth weight can serve as a predictor of their chances of survival. 13
Improved neonatal care has been made possible by technological advances and system coverage, which has increased the survival rate of preterm infants with very low birth weight. However, this has also increased the danger of developing severe ROP, which can result in partial or complete blindness. Since up to 90% of preterm birth retinopathy cases are preventable, early detection and treatment are crucial.14
Pulmonary Complications Associated with Mechanical Ventilation in the Critically Ill Neonate
Neonatal ventilation difficulties are more likely as time continues, but they also depend on the characteristics of the patient, the experience of the medical team, and the resources available. Peak pressure causes the airway to be injured, while high volume extends the socket, causing the injury to worsen. When healthy lungs are initially placed in an improper ventilation mode, the structure and function of the lungs can be significantly altered, which can lead to lung disease. Two terminologies are used to distinguish between these processes: ventilator-induced lung damage (VIL) and ventilator-associated lung injury (VALI). Differences in transpulmonary pressure, which result from an imbalance between pulmonary tension and stress, are the leading cause of lung injury in both situations. According to Carballo et al., airway-related pneumonia, pneumothorax, and bronchopulmonary dysplasia are among the respiration-related entities to which infants who need mechanical respiratory support are susceptible.15
Interpretation of Risk Factors Related to Central Venous Catheter Infections in Critically Ill Neonates
Based on the findings of the literature review, risk factors for central venous catheter infections were interpreted. We found that these risks are related to health professionals and the characteristics of newborns who require central vein catheter implantation as a necessary invasive procedure at the time of admission to intensive care units. These factors can also introduce mechanical and infectious complications. It was also determined that more databases on the management and prevention of infections through the use of catheters should be available, as these devices are very useful in critical neonatal settings where medical professionals need to be well-informed in the management and correct placement of catheters to reduce the risk of infection during a hospital stay.16
Risk Factors Associated with Low Birth Weight in Term Infants in Adolescent Pregnancy
Anemia and iron deficiency are two of the most common nutritional problems in the population, especially among disadvantaged people in developing countries. Pregnant women are classified into these groups because of increased iron requirements during pregnancy, which can account for up to one-third of all maternal stores. A 2015 study by Urdaneta et al., conducted in Chile, found a connection between anemia and low birth weight in infants.17
Stress During Pregnancy as a Risk Factor for Low Birth Weight
Stress during pregnancy has been shown to be a risk factor for low birth weight, increasing the chance of the newborn experiencing this problem by up to 5.6 times. Perceived stress, as a result of work problems, emotional distress at the time, financial worries and a general feeling of "overload", was shown to be considerably higher in the group of low birth weight mothers.18
Risk Factors Associated with the Degree of Intraventricular Hemorrhage in Preterm Infants
The 1978 review article by Papile L. et al. and the 2011 Cervantes paper estimated the prevalence of some degree of intraventricular hemorrhage in preterm infants younger than 36 years of age to be 50%. This is higher than the international average, which estimates between 25% and 60% in the series that was carried out for this study. When compared to research conducted in Latin America, there is also a risk of HIV when discovered by them, as was the case with Ferreyra and associates between 1999 and 2004, who reported an incidence of 40%. When compared to national surveys, such as the one conducted in 2012 in Monterrey by Crevantes-Ruiz, where the prevalence was 62%, this result is more comparable. The prevalence of any degree of intraventricular hemorrhage in live births is 28.5 per 1,000 live births.19
Risk Factors Associated with Patent Ductus Arteriosus in Very Low Birth Weight Infants
The last 20 years have seen significant advances in neonatology, which has increased the survival rate of very low birth weight babies in neonatais intensive care units. Many of these babies are also premature and have restricted intrauterine growth, which exponentially increases their morbidity. Ductus arteriosus persistence is a common pathology in this age group that increases its incidence at a shorter gestational age and increases mortality when it becomes hemodynamically significant.
Numerous complications and sequences affecting the respiratory system can arise in patients with hemodynamically significant ductus arteriosus. These include pulmonary edema, respiratory failure, pulmonary hemorrhages, prolonged time on mechanical ventilation, inability to extubate, apnea, and chronic premature lung disease.20
Risk Factors and Bronchopulmonary Dysplasia in Very Low Birth Weight Preterm Infants
Bronchopulmonary dysplasia has been determined to be associated with extremely preterm and extremely low birth weight. The incidence and severity of these conditions are inversely correlated with gestational age and birth weight. Low birth weight and shorter gestational age, according to previously published studies, are important risk factors for the development of this disease due to the incomplete structural development of the lungs, resulting in alveoli that are less flexible than their airways, increased alveolocapillary permeability, and lower activity of antioxidant and antiprotease enzymes. These factors increase the lung's susceptibility to injuries that limit lung function and the tissues' ability to heal the damage. Preterm infants are more likely to develop bronchopulmonary dysplasia when they have late neonatal sepsis and a systemic inflammatory response, according to several studies.21
Preterm and low birth weight newborns face an amalgam of risk factors that increase their vulnerability, creating a fertile ground for a range of medical complications. Prematurity, defined by birth before 37 weeks of gestation, stands as one of the main triggers of this situation. The lack of time for the full development of vital organs directly contributes to an increased risk of complications in these neonates.
Low birth weight, characterized by a weight of less than 2.5 kilograms, adds to the complexity of the situation. This phenomenon can stem from both prematurity and intrauterine growth restriction, where the placenta does not adequately provide the nutrients and oxygen needed for healthy fetal development. Placental dysfunction and problems in uterine circulation emerge as additional risk factors, intensifying the possibility of complications.22
Maternal infections during pregnancy, from urinary tract infections to systemic infections, are another facet of risk. These can increase the risk of preterm birth and adversely affect the fetus. In addition, extreme maternal age, whether in adolescence or at advanced ages, has been associated with an increased risk of preterm birth and complications in the newborn.23
The harmful influence of tobacco and toxic substances during pregnancy stands out as another significant risk factor. These habits increase the likelihood of preterm birth and contribute to adverse effects on fetal development. Multiparity, or having multiple pregnancies, is also presented as a risk factor, along with low socioeconomic status, which can translate into poor antenatal care, insufficient nutrition, and stress associated with lack of resources.
Medical complications affecting preterm and low birth weight infants are equally diverse and serious. Respiratory problems feature prominently, as lung immaturity can trigger respiratory distress syndromes, requiring interventions such as surfactant administration and mechanical ventilation. Cardiovascular complications, such as persistent pulmonary hypertension and heart failure, manifest due to immature cardiovascular function.24
Sensorineural complications, including brain bleeds, cerebral palsy, and cognitive developmental disorders, are an additional concern. Feeding and nutrition problems, with weak sucking and lack of sucking and swallowing reflexes, as well as feeding intolerance, affect the nutrition and growth of the neonate. The immaturity of the immune system increases the risk of infections, which can lead to sepsis and other infectious complications.
The challenge of maintaining an adequate body temperature, crucial for thermal homeostasis, is a common complication. Retinopathy of prematurity, an eye condition that affects vision, occurs most often in these infants. In addition to medical complications, parents of preterm infants face psychosocial difficulties, experiencing emotional stress and challenges related to the unpredictability of preterm birth and the complexities of neonatal care.25
Thus, risk factors and complications in preterm and low birth weight infants are intertwined in a complex web. A thorough understanding of these elements is crucial to implementing effective preventive and therapeutic interventions that address both the underlying causes and immediate consequences, thereby improving the prospects of these vulnerable neonates.
The situation of preterm and low birth weight infants is characterized by a complex web of risk factors that contribute to a range of medical complications. Prematurity, low birth weight, placental problems, maternal infections, harmful lifestyle habits, and low socioeconomic factors are intertwined to increase the vulnerability of these infants from the beginning of their lives.
The resulting medical complications run the gamut from respiratory and cardiovascular problems to sensorineural complications, infections, and challenges in food and nutrition. The immaturity of the organs and systems in these infants imposes a significant burden that requires specialized medical attention, precise interventions, and intensive care.
Despite these challenges, advances in neonatal medicine and developmentally focused approaches to care have significantly improved survival rates and long-term prognosis for these babies. However, the importance of prevention, quality antenatal care, and ongoing research to improve interventions and ensure the best possible outcome for preterm and low birth weight infants remains. Collaboration between health professionals, families, and communities is essential to address this complex reality and provide comprehensive support that promotes the health and well-being of these at-risk infants.
None.
This Review Article received no external funding.
Regarding the publication of this article, the authors declare that they have no conflict of interest.

