Preterm newborns (PTNB), especially those with a gestational age (GA) less than 28 weeks and/or birth weight less than 1250 grams, represent an extremely vulnerable population, with high rates of morbidity and mortality.1 In recent decades there has been an increase in survival in this population, but with greater morbidity, highlighting the deficits in neuropsychomotor development (NPD) and weight and height growth.2,3 The mortality frequency of these patients is around 40%, and approximately 25% of survivors evolve with cerebral palsy or some type of deficit in growth and/or NPD.2 The first 72 hours of life of the PTNB represent a stage of extreme vulnerability, due to the intense hemodynamic changes from the transitional period to extrauterine life.4 This phase is marked by an increased risk of irreversible brain damage, treatment-refractory hemodynamic instability and also an increased chance of death.4
Thus, in addition to aiming for survival and its increase for extreme PTNB, one of the great challenges in the Neonatal Intensive Care Unit is to contribute to the best possible quality of life for them, minimizing neurological comorbidities. In this context, infrared spectroscopy, also known as NIRS (Near-infrared spectroscopy®), has been applied as a method of monitoring regional oxygen saturation, and is currently applied mainly for cerebral, renal and/or mesenteric monitoring, depending on the patient's clinical need. The NIRS consists of a small equipment, which can be used at the bedside, it is a non-invasive method that allows continuous measurement/monitoring of regional oxygen saturation, that is, of a specific region of the body.5
Among the possible etiologies of neurological injuries that can affect PTNB, especially those with extremely low birth weight, are intraventricular hemorrhage and periventricular leukomalacia. Both are multifactorial, and the hypoxic-ischemic lesion is an event with a great impact on the future development of these newborns. This lesion reflects an imbalance between oxygen supply and demand in a certain brain region.6 Unfortunately, currently, neurological lesions in PTNB are diagnosed late, without the possibility of instituting early therapy and avoiding sequelae that can have an impact throughout the child's life. Continuous monitoring of cerebral oxygen saturation can be useful in early identification of a state of cerebral hypoxia or hyperoxia, which would hardly be identifiable only through clinical signs and symptoms.6
The hemodynamic evaluation of extreme PTNB is limited in our country, and clinical parameters/signs routinely used, such as blood pressure, are unspecific in this population and there is no consensus on the definition of hypotension for these neonates,7,8 impairing the assessment and early detection of problems related to specific/local oxygen saturation. However, there are few studies so far applying the NIRS in neonatology, especially in extremely low weight PTNB. This monitoring seems to be reliable to assess the hemodynamic status of PTNB, mainly because it is an extremely valuable hemodynamic parameter, which can be obtained in a non-invasive and continuous way.9
Through the application of this non-invasive and easy-to-apply method at the bedside, it may be possible to identify early hemodynamic instability and regional oxygen saturation, in an attempt to prevent and/or avoid brain injuries. But regional oxygen saturation (rStO2) reference values for PTNB have not yet been defined.10 Thus, the main objective of this case series is to verify whether the application of NIRS in this age group interferes with the mortality outcome and, in future studies with a larger sample, to identify cut off points for the rStO2 of extremely low weight PTNB, in the various possibilities of its regional monitoring (brain; kidneys; mesenteric).
In this prospective pilot case series, PTNB with birth weight less than 1250 grams, admitted to the Neonatal Center of the Instituto da Criança, Hospital das Clínicas, Faculty of Medicine, University of São Paulo, from September to November 2018, were included. Those who met the inclusion criteria (newborns with birth weight less than 1250 grams, born during the study period) were continuously monitored with the NIRS, regarding the measurement of cerebral and renal rStO2. Informed consent form was signed by the legal guardian for each newborn.
Monitoring protocol: performed in the first 24 hours of life; closed after completing 72 hours of monitoring. This period was chosen as it is the period of greatest vulnerability of blood flow and SpO2. The values found for cerebral and renal rStO2 were blinded and not reported to the medical team. Only the monitoring quality signal was exposed. Cerebral and renal rStO2 values were revealed only at the end of the research so that the PTNB would not undergo interventions based on rStO2 values, since the values are not yet fully defined in the scientific literature and so there is no bias regarding the outcome evaluated in this pilot: comparison of the frequency of those who died versus survivors, as well as determination of rStO2 cutoff points as a risk factor for increased mortality. The epidemiological characterization of the sample was performed using clinical data from each PTNB, obtained through the analysis of the electronic medical record (MV Soul).
Survival in the first 28 days of life was considered the primary outcome of this study. Patients who were transferred to other institutions, were born with congenital malformations that could cause hemodynamic changes, malformations of the central nervous system or who required surgery within the first 72 hours of life were excluded from the study. Gestational age was determined by the date of last menstruation (DLM) or obstetric ultrasound. Small for gestational age was defined as birth weight less than the 10th percentile for gestational age on the Fenton scale. Positive pressure ventilation in the delivery room was administered via a T-piece resuscitator. The SNAPPE II and CRIB II scales were used to measure the severity of clinical cases.
The results are presented in number with proportions (%), mean with standard deviation of the mean (SD) or median with interquartile range (IQ25%-75%). Comparisons between groups (death versus survivors) were performed using the Mann-Whitney test for continuous variables. All analyzes were conducted using IBM SPSS Statistics for Macintosh® software, Version 25.0. It was considered statistically significant when p ≤ 0.05.
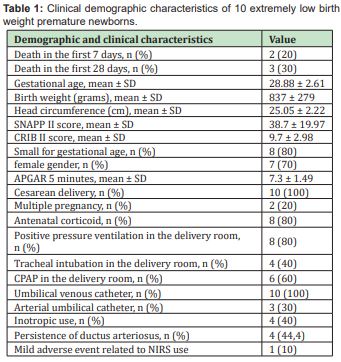
During the study period, 10 extremely low weight PTNB were included Table 1. Mortality in the first 28 days of life was 30%. Seven PTNB were female, with a mean gestational age of 28.88 ± 2.61 weeks and mean birth weight of 837 ± 279 grams. Of these, two PTNB were multiple pregnancies, eight were classified as small for gestational age (SGA); eight out of 10 received antenatal corticosteroids and in the 10 cases the delivery was cesarean. There was no use of epinephrine in the delivery room and no cases of chorioamnionitis were identified.
No serious adverse events related to the use of NIRS equipment were observed. There was only one mild adverse event in a newborn who presented mild hyperemia at the device's contact site, and it was not necessary to interrupt its use, the hyperemia disappeared after removing the electrode from the equipment.
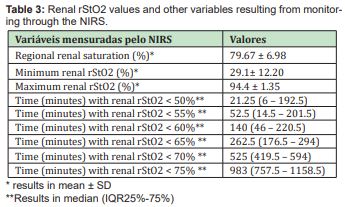
The values referring to regional cerebral oxygen saturation are described in Table 2. The mean regional cerebral oxygen saturation was 78.32 ± 6.77%. The values referring to regional renal oxygen saturation are described in Table 3. The mean regional renal oxygen saturation was 79.67 ± 6.98%.
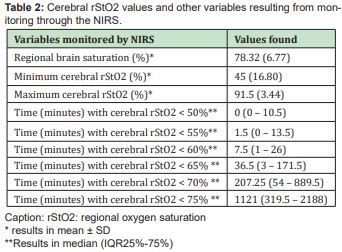
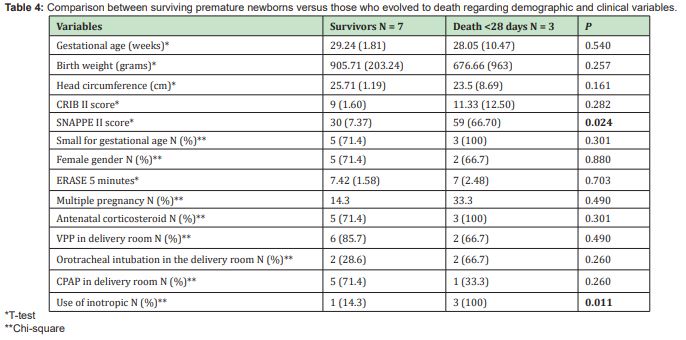
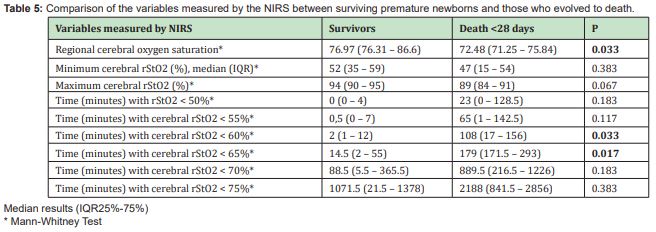
The comparison between the clinical characteristics and mortality of the sample are shown in Table 4. In a univariate analysis, it was possible to demonstrate that the SNAPPE II score is directly related to mortality (p=0.024), as well as the use of inotropic agents. related to higher mortality (p=0.011). Comparison of cerebral NIRS variables between surviving premature newborns versus those who evolved to death are shown in Table 5. The median regional cerebral oxygen saturation of surviving premature newborns was 76.97 (76.31 – 86.6), statistically higher compared to premature infants who evolved to death 72.48 (71.25 – 75.84), (p=0.033). The time in minutes with regional cerebral oxygen saturation less than 60% was significantly longer in newborns who died (p=0.033). The time in minutes with regional cerebral oxygen saturation less than 65% was significantly longer in premature newborns who died (p=0.017). There was no statistically significant difference regarding the time in minutes with regional cerebral oxygen saturation less than 70% between the groups (p=0.183).
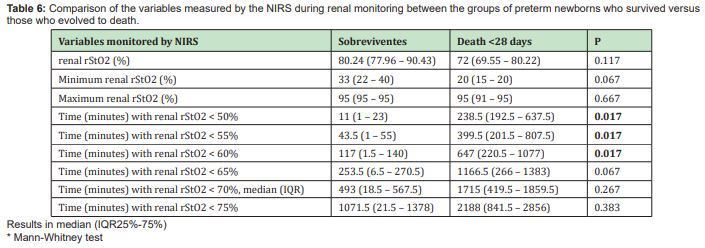
Comparison of the variables measured by the renal NIRS between the survivors and death groups are shown in Table 6. There was no statistically significant difference in the median value of regional renal oxygen saturation between the groups (p=0.117). The time in minutes with regional renal oxygen saturation less than 50% was significantly longer in preterm newborns who died compared to those who survived (238.5 vs 11 minutes; p=0.017). O tempo em minutos com saturação de oxigênio renal regional menor que 55% foi significativamente maior nos preterm newborns que foram à óbito (399.5 vs 43.5 minutos; p=0.017). The time in minutes with regional renal oxygen saturation less than 60% was significantly longer in preterm newborns who died (647 vs 117 minutes; p=0.017). There was no statistically significant difference regarding the time in minutes with regional renal oxygen saturation less than 65% between both groups (p=0.183).
To our knowledge, this is the first study to evaluate the use of infrared spectroscopy in very low birth weight preterm newborns in Brazil. With the data of these 10 pilot cases, it was possible to observe that in preterm newborns with very low birth weight that a lower cerebral rStO2 is associated with higher mortality in the first 28 days of life. This demonstrates that the NIRS can be useful, mainly because it is a non-invasive and continuous monitoring device, which allows the early identification of measures to increase cerebral rStO2 and can reduce the mortality of preterm newborns with birth weight less than 1250 grams. Classically, values between 55 to 85% have been used as a normality reference for cerebral rStO2. There are no studies to date validating these values for very low birth weight preterm newborns. In this case report, preterm infants who spent more time with cerebral rStO2 lower than 65% had a higher risk of death. However, the same cannot be said when the adopted value was less than 55%. A possible explanation for this data is that perhaps a cerebral rStO2 lower than 55% is too low a value, and it is enough to be lower than 65% to cause irreversible damage to the patient. However, more studies, especially randomized controlled trials, are needed to confirm these findings. But, without a doubt, this is an alarming fact that if confirmed, it proves that we are being permissive in relation to the value of cerebral rStO2. Adopting a safety band with a higher minimum cerebral rStO2 value (example: 65%) may be beneficial for the very low birth weight premature newborn.
Regarding renal rStO2, there was no statistically significant difference in its value between the survivors and non-survivors. However, very low birth weight preterm newborns who spent a longer time with renal rStO2 lower than 60% had a higher risk of death. This demonstrates that, perhaps, renal rStO2 can also be used as a marker of mortality in these patients. A descriptive analysis of cerebral and renal rStO2 values is necessary to understand the characteristics of this population, in order to offer a better treatment. Some limitations of the study should be considered when interpreting the results: small sample (n=10), which can make interpretation of the results difficult; there was no follow-up of these patients to assess neuropsychomotor development and correlate with mid- and long-term cerebral rStO2 values.
Normal values for cerebral rStO2 defined as 55 to 85% may not be beneficial for very low birth weight preterm infants. In this series of 10 cases, it was observed that a cerebral rStO2 lower than 65% is associated with higher mortality. It is necessary to define normal values of cerebral and renal rStO2 for very low birth weight preterm newborns. It is suggested that future studies be carried out correlating regional cerebral saturation values and short-, medium-, and long-term comorbidities.
None.
None.
The author declared no conflicts of interest.
- 1. Stoll BJ, Hansen NI, Bell EF, et al. Neonatal Outcomes of Extremely Preterm Infants From the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–456.
- 2. Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8(1):110–124.
- 3. Ancel PY, Goffinet F, Kuhn P, et al. Survival and morbidity of preterm children born at 22 through 34weeks’ gestation in france in 2011 results of the EPIPAGE-2 cohort study. JAMA Pediatr. 2015;169(3):230–238.
- 4. Rabe H, Rojas Anaya H. Inotropes for preterm babies during the transition period after birth: Friend or foe?. Arch Dis Child Fetal Neonatal Ed. 2017;102(6):F547–F550.
- 5. Wolf M, Greisen G. Advances in Near-Infrared Spectroscopy to Study the Brain of the Preterm and Term Neonate. Clin Perinatol. 2009;36(4):807–834.
- 6. Greisen G, Leung T, Wolf M. Has the time come to use near-infrared spectroscopy as a routine clinical tool in preterm infants undergoing intensive care?. Philos Trans R Soc A Math Phys Eng Sci. 369(1955):4440–4451.
- 7. Dempsey EM, Barrington KJ, Marlow N, et al. Management of hypotension in preterm infants (The HIP Trial): A randomised controlled trial of hypotension management in extremely low gestational age newborns. Neonatology. 2014;105(4):275–281.
- 8. Giesinger RE, McNamara PJ. Hemodynamic instability in the critically ill neonate: An approach to cardiovascular support based on disease pathophysiology. Semin Perinatol. 2016;40(3):174–188.
- 9. Janaillac M, Beausoleil TP, Barrington KJ, et al. Correlations between near-infrared spectroscopy, perfusion index, and cardiac outputs in extremely preterm infants in the first 72 h of life. Eur J Pediatr. 2018;177(4):541–550.
- 10. Greisen G, Gluud C. Cerebral near-infrared spectroscopy monitoring for prevention of brain injury in very preterm infants. Cochrane Database Syst Rev. 2017;4;9(9):CD011506.

