Background: Heart rate variability (HRV) is an indicator of autonomic activity in the regulation of circulation and changes have been associated with several pathological conditions.
Aims: The aim of the study was to acess the HRV as a predictor of extubation failure in pediatrics.
Methods: In this prospective observational pilot study, we included all consecutive patients from 1 month to 18 years of age who were admitted to the PICU in the ICr-HCFMUSP, São Paulo - Brazil. They were submitted to the spontaneous breathing test (SBT) and evaluated by HRV by the time and frequency domain variables derived from the Polar V800 equipment and the Kubios HRV Standart® program.
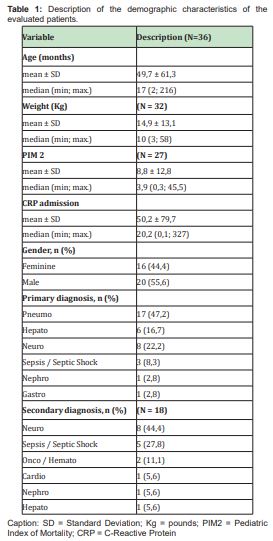
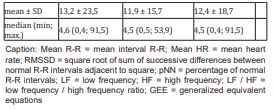
Results: A total of 36 patients [age 17 (2-216) months; male/female: 20/16; PIM2 3.9 (0.3-45.5); CRP (C-reactive protein) 20.2 (0.1-327); time of mechanical ventilation 5.0 (1.0-64.0) days] were included the study. The main diagnoses were 17 patients with lung diseases, 06 liver diseases, 08 neurological diseases, 03 sepsis/ septic shock, 01 nephropatic and 01 gastric disease. The data analyzed on HRV described in Table 3.
Conclusions: From the data analyzed, it can be concluded that the analysis of heart rate variability was not a predictor of success/failure of tracheal extubation for the pediatric sample studied.
Breathing is one of the fundamental foundations of human life, necessary for survival and related to the intrinsic mechanism of the respiratory system. Ventilatory insufficiency is the inability to maintain the effective exchange of oxygen (O2) and carbon dioxide (CO2).1 Mechanical ventilation (MV) is a frequent procedure for ventilatory support in patients with acute ventilatory insufficiency (IVA). It is invasive, expensive, and linked to potential risks (pneumonia, pulmonary injury associated with MV, hemodynamic changes, decreased respiratory muscle strength and endurance, and prolonged ICU stay).1-4 Ventilatory weaning in pediatric patients is desirable and should be started 24 hours after orotracheal intubation (OTI).5-7 The process of withdrawal from ventilatory support occupies about 40-50% of the total time of MV.8,9 Weaning protocols reduce MV time and ICU stay.2,10,11 The pathophysiology of ventilatory weaning failure is complex and involves the interaction between cardiorespiratory reserve, autonomic functioning and the musculoskeletal capacity of the individual.6,12 ICU patients generally present metabolic, endocrine, neurological, muscular and immunological alterations, which may alter the weaning time of MV.1,5,12 Early use of spontaneous ventilatory modes such as synchronized intermittent MV (SIMV) and supportive pressure ventilation (SPV) facilitates the weaning process of MV and tracheal extubation. These modes are well tolerated by most pediatric patients and allow shorter MV time and earlier extubation.13,14
The spontaneous breathing test (SBT) is considered one of the successful predictors of weaning and extubation.6 In the ICU, SBT is a common practice because it allows the assessment of children's cardiorespiratory tolerance during minimum ventilatory support.8,9 The sensitivity of SBT is 83% to recognize children who have a chance of successfully withdrawing ventilatory support. Thus, there is a higher proportion of successful extubations than failures.8 The reintubation rate is related to the increased morbidity and mortality of ICU patients.15 Methods of cardiorespiratory behavior analysis have been applied in clinical studies of ventilatory weaning and tracheal extubation, which demonstrate that healthy biological systems have innate and highly complex patterns of cardiorespiratory variability. However, when these systems present conditions, the variability is altered and the complexity reduced. This decrease is indicative of reduced adaptability, reflects changes in cardiorespiratory systems and has been described as a marker of results in several clinical situations. Cardiorespiratory variation is related to the balance of the sympathetic and parasympathetic systems of the thermal, respiratory and cardiac control functions.11,16-19
The assessment of heart rate variability (HRV) has been a predictor of success in ventilatory weaning in adult patients.5,11,19,20 The combination of cardiorespiratory variation and clinical response to SBT had better accuracy of tracheal extubation success than any other predictor evaluated alone.14 A similar result was observed when applying cardiorespiratory variability in the neonatal population.19,21 However, there are not published studies on HRV in the pediatric population related to ventilatory weaning and tracheal extubation. Therefore, the aim of this study was to verify the applicability of HRV as a predictor of failure / success of tracheal extubation in the pediatric population.
This prospective cross-sectional clinical trial, including a convenience sample of patients admitted to the PICU of FMUSP, from November 2017 to July 2018. We evaluated children of both genders, aged between 30 days and 17 years, 11 months and 29 days of life. Study approved by the Institution (CEP nº 13.267/2015). Children undergoing MV for more than 24 hours and with clinical eligibility criteria for SBT22 were included; those with tracheostomy, with orotracheal tube escape (with or without cuff) ≥15% were excluded.
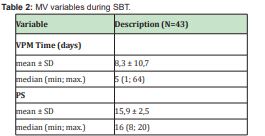
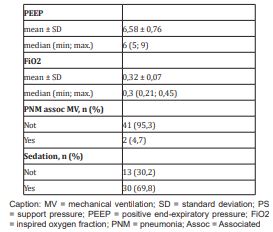
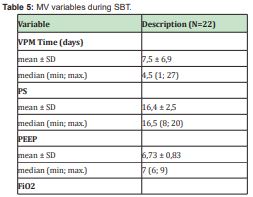
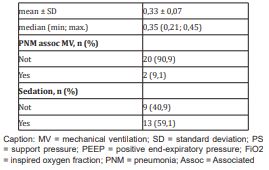
HRV analysis was applied throughout the SBT, which consisted of keeping the child breathing spontaneously, in the supportive pressure ventilation (PSV) modality for 60 minutes (according to the PICU pre-existing protocol). The ventilatory parameters used in this ventilatory modality were: support pressure (SP): 10-7cm H20; positive end-expiratory pressure (PEEP): 5-6cm H20; inspired fraction of O2(FiO2): the lowest possible for O2 saturation values (SpO2) ≥ 90%, provided it was ≤50%. The variables analyzed during the SBT were: HRV variables - time domain (mean RR, mean HR, RMSSD, pNN50) and frequency domain (LF, HF, LF / HF ratio). These data were collected at eight different times during the SBT: five minutes before the test; five, 15, 30, 45 and 60 minutes of test; five and 30 minutes after the end of the test. After recording these variables in the data collection form, the child was or was not elected for tracheal extubation; considering only the success criteria of SBT (maintenance of respiratory rate, cardiac rate and SpO2 stability; maintenance of minute volume during SBT; absence of use of accessory respiratory muscles during the test);22 HRV analysis data were not used to determine whether or not the child would be extubated. Statistical analysis of HRV variables was performed only after the completion of the weaning / extubation process of each patient.
Criteria for discontinuation of the study protocol were: variation of vital signs (HR, RF and BP) above or below 30% of predicted for age; SpO2 lower than 88% or need to increase FiO2 during test. The presence or absences of signs of respiratory distress were also considered, such as the use of accessory respiratory muscles, pallor, sweating and/or psychomotor agitation. In the presence of any changes mentioned above, the SBT was interrupted and the child returned to ventilatory mode prior to the test. After 24 hours of respiratory muscle rest, the child could perform a new SBT.22 To measure vital signs during SBT, the Dixtal® multiparametric monitors (DX 2010; DX 2023; 2022), present in each PICU bed, were used. For HRV data, Polar® V800 was used and their conversion using the Kubios HRV Standard® program. MV was performed using the following devices: E500 (Newport Medical Instruments®) and Servo I (Maquet Medical Instruments®).
The tests were performed by trained physical therapists. Data were entered into the SPSS 17.0 program and double-checked for consistency. For statistical analysis, the Kolmogorov-Smirnov (KS) test was used to adhere to the Gauss curve and to pair the sample. For the parametric variables, Student's t-test was used and the results presented as mean and standard deviation; nonparametric variables were analyzed using Fisher's chi-square test and presented as median (minimum-maximum) or median and interquartile ranges 25%-75%; variables with three or more measurements were analyzed by the one-way ANOVA test. HRV parameters were described according to extubation success using summary measures and verified the influence of these parameters on extubation success using generalized estimation equations (EEG) with binomial distribution and log it binding function, assuming an autoregressive correlation matrix of first order between attempts23. Microsoft Excel 2003 software was used for data tabulation and statistical analyzes were performed using IBM-SPSS® for Windows version 22.0 software; considering statistically significant when p≤0.05. Results are presented in tables.
In 2017 there were 571 hospitalizations in the PICU where data were collected for this research, and 221 (38.7%) patients received invasive ventilatory support with extubation failure of 10.8% (N = 24 children); in 2018 there were 565 hospitalizations with 205 (33.6%) patients undergoing invasive ventilatory support with extubation failure of 12.7% (N = 26 children). During this study (from November 2017 to July 2018) approximately 420 children were admitted to the PICU, of which 147 (35%) used invasive ventilatory support and 55 patients were considered eligible for SBT, and 36 patients met the criteria of inclusion for this study. During this study period, extubation failure occurred in 11% (N = 16 children) of the total sample of 147 children undergoing invasive ventilatory support. During the study period, 55 patients were eligible for SBT. Of these, 19 were excluded due to the following reasons: 12 due to non-signature of the consent form due to the absence of the presence of legal guardians before data collection for this research; five (05) due to interference with the Polar® monitor signal during SBT; two (02) due to having performed T-tube SBT. In the study, included 36 patients, 43 SBT were performed, since five patients required more than one SBT during PICU admission to present clinical conditions for extubation. The epidemiological data of the total study sample are presented in Table 1, just as the variables of MV are in Table 2. Failure and successful extubation groups were compared for HRV parameters (Table 3), in which it was observed that there was no statistically significant difference between them. By identifying the most frequent subgroup in this study by clinical diagnosis, it was observed that 47.2% of the sample cosnsisted of patients with a primary diagnosis of respiratory cause (Table 1), whose demographic and ventilatory characteristics are presented in Tables 4 and 5. When comparing the extubation success versus failure groups specifically for this subgroup, it was also observed that there was no statistically significant difference for HRV variables (Table 6).
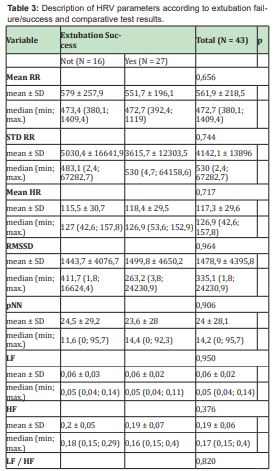
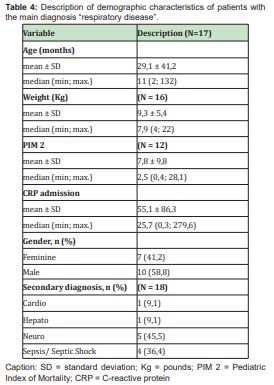
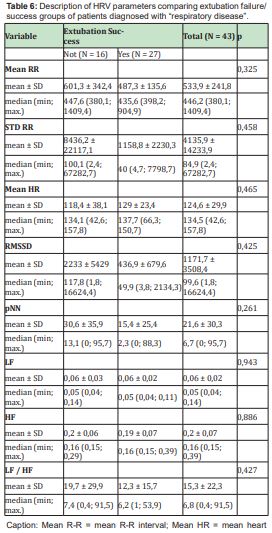
The present study aimed to verify whether HRV is a predictor of success/failure of tracheal extubation in pediatrics. The main results were that HRV was not a predictor of success/failure of tracheal extubation in this sample, not even when the analysis occurred in the subgroup “respiratory disease” (higher number of hospitalized patients in the analyzed period - 47.2%). It is possible to determine a cutoff point for HRV variables for this group of patients. Determining the optimal time to start ventilatory weaning remains a major challenge in PICU. Long term MV stay is associated with important complications such as pneumonia and changes in muscle strength and endurance, increased morbidity and mortality. However, it is known that early weaning can be harmful to patients, especially in the pediatric population.24 Ventilatory weaning/tracheal extubation protocols aim to reduce MV time and ICU stay.6,25,26 A standardized approach to managing the management of the ventilatory weaning process contributes to reducing MV time and improving clinical outcomes for the patient.24,27 For the discontinuation of ventilatory support, decision-making is expected to be based on tests, criteria and objectives that determine the appropriate time for its initiation and completion with the success of tracheal extubation.24,28 The most frequently used strategy for ventilatory weaning of infants and children is clinical judgment and the gradual reduction of ventilatory parameters. Extubation is usually performed based on minimum ventilatory support parameters or after SBT.29
Several studies30-34 discuss the optimal duration of SBT, and some have previously shown that SBT lasting between 30 minutes and two hours was sufficient to consider patients fit or not for tracheal extubation. In our study, the SBT time was 60 minutes and was performed in PSV ventilatory mode, according to institutional protocol. Cardiovascular changes can be assessed in several ways, including HRV analysis. The study of HRV is a noninvasive and selective method that evaluates autonomic modulation.35,36 This analysis demonstrates the interaction of the sympathetic and parasympathetic autonomic system in the face of different clinical situations, such as the presence of respiratory and/or neurological diseases and/or routine ICU procedures, such as respiratory physiotherapy and ventilatory weaning.35,36 Marsilio L et al, 201937 conducted an observational study with 17 children in a university hospital (age 1.21 [0.28; 14.81] years) and evaluated their HRV in the first 24 hours of stay in the PICU and in the last 24 hours after the resolution of the underlying disease. As in our study, the time domain variables were evaluated: RMSSD, pNN50 and SDNN and from the collected data, concluded that HRV is a marker of recovery in severely ill children, considering that HRV significance was observed at to compare the data of the first with the last 24 hours of the child's stay in PICU.37 The instability of the autonomic system occurs before the deterioration of clinical signs or the results of laboratory tests in newborns (NB),38 which also seems to occur in the pediatric age group.37
The study by Kaczmarek J et al 201338 compared HRV differences between NB (N = 47 NB; weight ≤ 1,250 grams) successfully versus tracheal extubation failure, as well as assessing HRV accuracy as a predictor of tracheal extubation readiness. They concluded that infants who failed the first attempt at tracheal extubation had a reduced HRV during SBT.38 Neural mechanisms are responsible for regulating inflammation, so the literature suggests an association between HRV and inflammation/infection.39,40 Respiratory infections, such as pneumonia and bronchiolitis, which are common in children, trigger an inflammatory process with release of specific inflammatory mediators (bronchiolitis → IL8; pneumonia → C-reactive protein - CRP).39,40 Marsland AL et al41 demonstrated that decreased vagal activity is associated with increased inflammation, as Sloam et al40 found results confirming the hypothesis that lower vagal activation is related to increased proinflammatory cytokine production. These are present in many different inflammatory processes, such as respiratory diseases, however, this information has not been studied in the pediatric population. Based on this information, the prospective study by Jacinto CP42 aimed to assess changes in HRV resulting from impaired cardiac autonomic performance in infants diagnosed with acute viral bronchiolitis (AVB). We included 24 children (mean age 6±2 months) subdivided into two groups (control: no respiratory disease; intervention: with AVB). From the results obtained, they concluded that respiratory physiotherapy and nasotracheal aspiration, both used for airway clearance, promote improvement in HRV autonomic modulation in infants diagnosed with AVB.42
In our study, HRV was not a predictor of tracheal extubation failure/success, even when the subgroup “respiratory disease” was analyzed. This result is believed to be due to the heterogeneous pediatric population studied (mean age 49.7±61.3; mean weight 14.9±13.1; CRP admission 50.2±79.7). The maturation of the sympathetic and parasympathetic systems is known to accompany the child's growth. Therefore, there is a growing increase in autonomic modulation in the pre and postnatal periods.42 This factor may have contributed to the fact that HRV was not statistically significant as a predictor of tracheal extubation failure/success. The absence of previous studies in pediatrics with subgroup analysis for specific diseases / pathophysics make it difficult to compare behavior in the process of ventilatory weaning/tracheal extubation in this age group.36,42 In general, the studies are based on short-term HRV records and involve heterogeneous groups with divergent results.36,42
Thus, our study was unable to detect HRV influences as a determinant of extubation success/failure in the sample studied, specifically in those diagnosed with respiratory disease. However, some limitations of the study may have interfered with the results, such as: age heterogeneity and small sample size (although previous studies included around 20 children). The continuity of this study is necessary to confirm the findings from the analysis of 43 SBT.
From the data analyzed, it can be concluded that the analysis of heart rate variability was not a predictor of success/failure of tracheal extubation for the pediatric sample studied. The continuity of the study is suggested to confirm the findings.
None.
The author declared no conflicts of interest.
- 1. Dixit A, Prakash S. Effects of threshold inspiratory muscle training versus conventional physiotherapy on the weaning period of mechanically ventilated patients: a comparative study. Int J Physiother Res. 2014; 2(2):424–428.
- 2. Kirakli C, Ediboglu O, Naz I, et al. Effectiveness and safety of protocolized mechanical ventilation and weaning strategy of COPD patients by repiratory therapists. J Thorac Dis. 2014;6(9):1180–1186.
- 3. Estebán A, et al. A comparison of four methods of weaning patients from mechanical ventilation. The New England Journal of Medicine. 1995;332(6):345–350.
- 4. Silva DCB, Shibata ARO, Farias JÁ, et al. How is mechanical ventilation employed in a pediatric intensive care unit in Brazil? Clinics. 2009;64(12):1161–1166.
- 5. Huang CT, Tsai YJ, Lin JW, et al. Application of heart-rate variability in patients undergoing weaning from mechanical ventilation. Critical Care. 2014;18(R21):1–9.
- 6. Hayashi LY, Gazzotti MR, Vidotto MC, et al. Incidence, indication and complications of postoperative reintubation after elective intracranial surgery. Sao Paulo Med J. 2013;131(3):158–165.
- 7. Nemer SN, Carmen Sílvia Valente Barbas CSV. Predictive parameters for weaning from mechanical ventilation. J Bras Pneumol. 2011;37(5):669–679.
- 8. Andrade LB, Melo TMA, Morais DFN, et al. Avaliação do teste de respiração espontânea na extubação de neonatos pré-termo. Rev Bras Ter Intensiva. 2010;22(2):159–165.
- 9. Valenzuela J, Araneda P, Cruces P. Weaning from Mechanical Ventilation in Pediatrics. State of the Art. Arch Bronconeumol. 2014;50(3):105–112.
- 10. Zeggwagh AA, Abouqal R, Madani N, et al. Weaning from mechanical ventilation: a model for extubation. Intensive Care Med. 1999;25:1077–1083.
- 11. Seely AJE, et al. Do heart and respiratory rate variability improve prediction of extubation outcomes in critically ill patients? Critical Care. 2014;18(R65):1–12.
- 12. Verceles AC, Diaz-Abad M, Geiger-Brown J, et al. Testing the prognostic value of the rapid shallow breathing index in predicting successful weaning in patients requiring prolonged mechanical ventilation. Heart & Lung. 2012;41:546–552.
- 13. Glover G, Connolly B, Gangi SD, et al. An observational cohort study to determine efficacy, adherence and outcome of the early initiation of pressure support ventilation during mechanical ventilation. BMJ Open Resp Res. 2014;1:e000028.
- 14. Sant´Anna GM, Keszler M. Weaning infants from mechanical ventilation. Clin Perinatol. 2012;39:543–562.
- 15. Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcme of mechanical ventilation. Chest. 1997;112:186–192.
- 16. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996; 93(5):1043–1065.
- 17. Perini R, Veicsteinas A. Heart rate variability and autonomic activity at rest and during exercise in various physiological conditions. Eur J Appl Physiol. 2003;90:317–325.
- 18. Malpas SC. Neural influences on cardiovascular variability: possibilities and pitfalls. Am J Physiol Heart Circ Physiol. 2002;282:6–20.
- 19. Precup D, Robles Rubio CA, Brown KA, et al. Prediction of extubation readniness in extreme preterm infants based on measures of cardiorespiratory variability. 34th Annual International Conference of the IEEE EMBS. 2012; pp. 5630–5633.
- 20. Shen HN, Lin LY, Chen KY, et al. Changes of heart rate variability during ventilator weaning. Chest. 2003;123:1222–1228.
- 21. Kaczmarek J, Chawla S, Marchica C, et al. Heart rate variability and extubation readiness in extremely preterm infants. Neonatology. 2013;104:42–48.
- 22. Johnston C. Índices preditivos de desmame e extubação. In: Barbosa AP, Johnston C, Carvalho WB. Desmame e extubação em pediatria e neonatologia. São Paulo: Atheneu. 2010. pp. 111–128.
- 23. McCULLAGH P, NELDER JA. Generalized linear models. New York: Chapman and Hall. 1989. p 511.
- 24. Ferreira FV. Avaliação da eficácia do teste de respiração espontânea na predição do sucesso da extubação no pós-operatório de cirurgia cardíaca em crianças: estudo randomizado-controlado. Tese de doutorado – USP. Ribeirão Preto/ SP. 2018. Pp. 49.
- 25. Zeggwagh AA, Abouqal R, Madani N, et al. Weaning from mechanical ventilation: a model for extubation. Intensive Care Med. 1999;25:1077–1083.
- 26. Seely AJE, et al. Do heart and respiratory rate variability improve prediction of extubation outcomes in critically ill patients? Critical Care. 2014;18(R65):1–12.
- 27. Boles JM, Bion J, Connors A, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29: 1033–1056.
- 28. McConville JF, Kress JP. Weaning patients from the ventilator. N Engl J Med. 2012;367(23):2233–2239.
- 29. Jonhston C, Silva PSL. Weaning and extubation in pediatrics. Current Respiratory Medicine Reviews. 2012;8:68–78.
- 30. Ely EW, Baker AM, Dunagan DP. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med. 1996;335:1864–1869.
- 31. Esteban A, Alia I, Tobbin MJ. Effects of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med. 1999;159:512-518.
- 32. Esteban A, Alia I. Clinical management of weaning from mechanical ventilation. Intensive Care Med. 1998;24:999–1008.
- 33. Matic I, Majeric Kogler V. Comparison of pressure support and T-tube weaning from mechanical ventilation: randomized prospective study. Croat Med J. 2004;45:162–166.
- 34. Perren A, Domenighetti G, Mauri S, et al. Protocol-directed weaning from mechanical ventilation: clinical outcome in patients randomized for a 30- min or 120-min trial with pressure support ventilation. Intensive Care Med. 2002;28:1058–1063.
- 35. Jonhston C, Piva J, Carvalho WB, et al. Post cardiac surgery In children: extubation failure predictor's. Rev Bras Ter Intens. 2008;20:57–62.
- 36. Southall DP, Scherchtman VL, Raetz SL, et al. Dynamic analysis of cardiac R-R intervals in normal infants and in infants who subsequently succumbed to the sudden infant death syndrome. Pediatr Res. 1992;31:606–612.
- 37. Marsilio LE, Manghi T, Carrolls MS, et al. Heart rate variability as a marker of recovery from critical illness in children. PLoS ONE. 2019;14(5):e0215930.
- 38. Latremouille S, Al Jabri A, Lamer P, et al. Heart Rate Variability in Extremely Preterm Infants Receiving Nasal CPAP and Non-Synchronized Noninvasive Ventilation Immediately After Extubation. Respiratory Care. 2018;63(1):62–69.
- 39. Abu-Harb M, Bell F, Finn A, et al. IL-8 and neutrophil elastase levels in the respiratory tract of infants with RSV bronchiolitis. Eur Respir J. 1999;14:139–143.
- 40. Sloan RP, McCreath H, Tracey KJ, et al. RR Interval variability is inversely related to inflammatory markers: the CARDIA Study. Mol Med. 2007;13(3-4):178–184.
- 41. Marsland AL, Gianaros PJ, Prather AG, et al. Stimulated production of proinflammatory cytokines covaries inversely with heart rate variability. Psychosomatic Medicine. 2007;69:709–716.
- 42. Jacinto CP, Gastaldi AC, Aguiar DY, et al. Physical therapy for airway clearance improves cardiac autonomic modulation in children with acute bronchiolitis. Braz J Phys Ther. 2013;17(6):533–540.

