Stroke is one of the leading causes of death in developed countries and can result in physical, sensory, and cognitive deficits. The aim of this study is to enunciate the perception of occupational therapists about the application of Bobath and PNF methods in the treatment of hemiplegic patients. It is intended to conduct a qualitative, descriptive, exploratory, and cross-sectional study, with 19 occupational therapists to practice in Physical Rehabilitation in Portugal. The results show that it is necessary to carry out training for the application of the methods under study. The combined use of techniques is the most adopted model, and therapists use them throughout the rehabilitation process.
In conclusion, Proprioceptive Neuromuscular Facilitation, being the least recognized in terms of effectiveness and Bobath, being the most used and in which therapists have more training, are the most used methods by occupational therapists. 1
Keywords: Stroke, Hemiplegia, Occupational therapy in physical rehabilitation, Bobath method, POP method
Stroke is one of the main causes of death in developed countries and, for the most part, resulting from a vascular occlusion that leads to the interruption of oxygen and glucose flow to the brain structures leading to the death of tissues, which results in somatosensory deficits, pain, visual and/or motor deficits, changes in muscle tone, existence of abnormal movement patterns, pathological reflexes, paresis, disturbances in posture and balance, speech and language, cognitive dysfunction, among others.1 The earlier the intervention process, the more likely it is to recover.2.3 The approach in Occupational Therapy (OT), aims to provide autonomy to people with specific problems (physical, sensory, psychological, mental, or social) presenting, for a temporary or definitive period difficulty in their occupational performance,4 aiming at promoting the health and well-being of patients, using various methods of intervention either in isolation or combined.5–7 Thus, the focus of the intervention in OT is to improve the performance of the patients in the various activities of daily life.8
Using several specific intervention techniques, the occupational therapist provides the patient with a relearning of voluntary control of the injured musculature, as well as the learning of new motor skills, through the performance of structured functional activities.9 The therapist should identify the barriers to their autonomy, facilitate the participation of individuals with disabilities in their activities of daily living and/or suggest changes in the environment that may favor it.5–7 Thus, it is important to conduct investigations that can guide clinical reasoning when selecting the methods to be used in the intervention process.
The methods under study, Bobath and PNF are two methods that can be used to improve the motor functionality of the hemiplegic patient, making it more autonomous in day-to-day activities. Bobath can be defined as a neuro developmental treatment technique widely used worldwide in the rehabilitation of hemiplegic individuals,10 and can be applied to all age groups as well as to any degree of functional disability.11 It uses the handling of targeted key control points to support the body segments as well as to assist the individual in achieving active body control. It also states that postural alignment and postural stability are facilitated when the tone is increased as well as minimizing abnormal movement patterns.12.13
This method uses in its approach, the normalization of muscle tone, minimizing primitive patterns, as well as facilitating automatic movement reactions and the normal movement pattern.14–16 It aims to achieve normal patterns of movement, normalization of the tone, control of head and trunk and to minimize abnormal movement patterns.2
For the application of this method, an in-depth knowledge about the normal sequential development of motor behavior is required.17 The method under study also encourages bilateral use of the body to model pathological motor patterns and provide a relearning of movements. It works on proximal joints stabilizing key points in the opposite patterns to the inadequate ones that predominate in the patient, to redirect them and promote appropriate motor standards.18
Corroborating its efficacy as well as the phase of evolution of clinical recovery of the patient in which the method is most used, we identify the studies previously conducted with the use of this concept, namely Physiotherapy based on the Bobath concept for adults with post-stroke hemiplegia: a review of effectiveness studies" whose purpose is to verify evidence to prove whether or not the Bobath method is effective in the treatment of individuals with hemiplegia, as well as whether it is the most effective when compared to other methods. The author said that the effectiveness of the Bobath method is questionable, as there is not enough scientific evidence to prove its efficacy or non-efficacy.10
The authors of the study "Rehabilitation after ischemic stroke in the elderly" state that the Bobath and PNF methods have improvements and are more effective in treating individuals after stroke in the elderly when compared to other traditional methods.2 The PNF or Proprioceptive Neuromuscular Facilitation method is an approach that combines patterns in motion diagonals based on neuromuscular facilitation techniques to provoke or facilitate motor responses and improve neuromuscular control and function. It is used to develop muscle strength and endurance, promote joint stability, mobility neuromuscular control, facilitate coordinated movements using the strongest movement patterns to strengthen weaker movement patterns, as well as the creation of pathways for the expression of functional movement patterns and their integration into the central nervous system (CNS) through manual stimulation and verbal instructions to induce patterns of thus improving motor function.16
It is a therapeutic resource of easy application, also used in patients who have suffered stroke,8 improving their quality of life19 and leading to an improvement in motor function, with no pain.20,21 Knott and Voss believed it was possible to alter or facilitate specific motor patterns through sensory stimuli, mainly by proprioceptive approach. This, in turn, would produce permanent effects on the CNS.22 The PNF benefits from basic procedures such as resistance (assists motor control, contraction and muscle strength), irradiation and reinforcement (generates the propagation of the stimulus and is usually used in an early stage of the rehabilitation process, as a preparatory technique), manual contact (promotes stimulation of sensory receptors, guides movement through touch and pressure), verbal command (guide, prepares and corrects movement), visual stimulus (guide, corrects and improves movement), traction and approximation (facilitates movement, stabilizing the limb), stretching (provides a muscle contraction and prevents fatigue), synchronization of movements and patterns (to highlight results and facilitate normal movement).20,23–25
In the study "Effects of proprioceptive neuromuscular facilitation (NPF) on the overall improvement of patients affected by stroke", the author concludes that the method is widely used in rehabilitation programs in the treatment of individuals with stroke and demonstrates gains in functionality, strengthening and relaxation of muscle groups, and it is necessary to master the technique for effective treatment. However, evidence is needed to prove that the exclusive application of the method is effective, as it is mostly applied jointly with other techniques.19
Both Bobath and PNF methods can be used throughout the rehabilitation process, however, the intervention must meet the needs of each patient, and should be systematically evaluated and reevaluated at each stage of the rehabilitation process. It is up to the occupational therapist to select the methods and techniques that best suit the patient.1 This study proposes to enunciate the opinion of occupational therapists about the use of these two methods of intervention in the rehabilitation process in hemiplegic patients. Specifically, it was intended to identify possible advantages and disadvantages over their application, the effectiveness of both in stroke, and the application of techniques considering the state of evolution of the hemiplegic patient in the rehabilitation process. The theme of the study was selected considering the insufficiency of studies on this area.
The study is qualitative, descriptive, exploratory, and cross-sectional.26 The variable under study deals with the perception of the occupational therapists about the application of the Bobath and PNF methods in stroke patients. The methodology of choosing the sample is convenience (or accidental),27 consisting of 19 occupational therapists to practice in the area of Physical Rehabilitation, who meet the following inclusion criteria:
- Experience in the practice of at least 3 years
- Intervention with adult patients affected by stroke
- Use, in its clinical practice, of at least one of the methods under study
- Practice your profession in Portugal
- Authorize the participation in the study by completing the Informed Consent
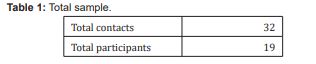
Based on Table 1, we can observe that 32 contacts were made to Occupational Therapists, and 19 positive responses were obtained (N=19).
Gender and age of participants
Figure 1 shows that of the 19 participants, 12 are female (63%) and 7 male (37%), the age of the participants varies between 25 and 63 years, with a mean of 30 years.
Year of graduation
Table 2 The interviewees perform functions in Physical Rehabilitation, most in Hospital Units, in hospitalization and outpatient clinics and the rest in Continuing Care Units and Private Clinics. Other interviewees who, in addition to practicing their clinical practice, are also teachers. The semi-structured interview with the informed consent of the participants was used as a data collection instrument, through the completion of the "Helsinki Declaration" of the World Medical Association. Data were collected from November 2021 to September 2022. In a first phase, a pilot study was conducted, through which one can perceive the feasibility of the script of the interview initially proposed.28 After making the necessary adjustments, 19 interviews were conducted and their contents were recorded for further analysis, with the consent of the interviewees. Then, its transcription was carried out. Finally, content analysis and discussion of the results obtained were performed.

The general reading of what is described in the previous tables suggests, for better appreciation, the creation of some transversal categories, namely Table 3:
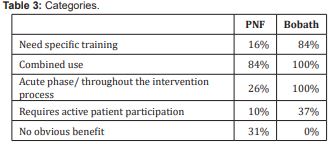
Specifically, and by exploring the different dimensions, it is possible to verify their relative weight. For better appreciation, the results presented refer to the Bobath method in isolation (I), to the PNF method in isolation (II) and to both (III) in the view of the respondents.
Use of the Bobath method in isolation
As stated on Table 4, 13 of the participants explain that academic training is needed for the application of the method: “(...) It is necessary to have a great knowledge of the method (...)".
Other 5 state that the application of the method “(...) requires a huge active participation of the patient (...)” Table 5.
Most occupational therapists (N=11) "(...) use at a more acute or subacute stage. At a later stage, they did not use Bobath so much (...)", and some of the interviewees (N=9) reported that "(...) I use Bobath throughout the intervention process (...)" Table 6.
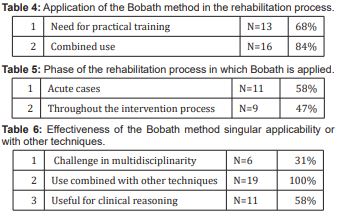
For some of the interviewees (N=6) the "(...) multidisciplinary teams (...) it is difficult to have an entire team working within the same concept (...)”.
All therapists (N=19) reported "(...) I use in conjunction with other techniques (...)".
Use of the PNF method in isolation
Table 7It was possible to verify in table 7 that 16 of the participants “(…) use this method in conjunction with other methods or techniques "(...) I use in conjunction with Panat (...), and rood for example(...)".
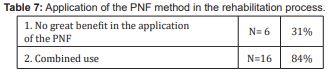
For some interviewees (N=6), "(...) personally I do not see advantages in neurological patients (...)". rehabilitation process in which PNF is applied
According to Table 8, 2 of the therapists said that they use PNF throughout the rehabilitation: "(...) I use PNF throughout the process (...)" Table 9.
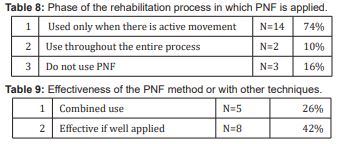
9 of them use it when there is already active movement: "(...) I only use PNF when there is already active movement (...)", and 3 indicated that: “(…) personally I see no advantage in neurological patients (…)”.
As is stated on table 9, 5 therapists indicate "(...) I use in conjunction with other techniques (...)", 2 show that "(...) all techniques are advantageous as if the patient's response is positive (...)".
3 of them say that “(…) if it is well applied, in a short time I can have significant improvements (…)”.
Use of both methods
Table 10In general, the interviewees (N= 8) reported that "(...) I think I've always seen results, now I can't say it was specifically for one or the other because I don't use one or the other in isolation (...)”.
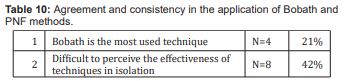
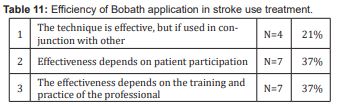
2 indicate that “(…) Bobath is the one that has been applied most (…)” Table 11.
For 4 therapists, "(...) the variety of neurological cases that we have is so large, that it is very difficult to have a homogeneous sample to prove that the concept is effective (...)”.
For 7 interviewees, the choice of the application of the techniques and their effectiveness depends directly on the participation and involvement of the patient, as well as on their own training, stating that "(...) I have not done specific training of any of the techniques. The effectiveness of the techniques also depends on the participation and involvement of the patient (...)".
Regarding the response time/evolution of the patient, for (N=5) they state that "(...) for me the Bobath method causes the person to evolve gradually and as normal as possible (...), (...) there turns out to be a much more fluid and linear evolution (...), (...) we see evolution, but there is no short-term and long-term evolution (...)". There is no consensus in the literature on the ideal duration of the rehabilitation process, nor at what time after stroke the method should be applied.10 However, early rehabilitation is beneficial and the use of the Bobath method also allows satisfactory results to be achieved,20 after a long period of evolution Table 12.
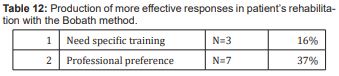
For the interviewees (N=7), it was possible to notice that the choice of the use of the concept, as an intervention method, comes from a personal preference "(...) I think it also has to do with professional preference and for me the concept of Bobath makes more sense (...)".
For (N=3) this decision also depends on your knowledge of the method as well as their working conditions "(...) It is necessary to have a great knowledge of the method as well as an appropriate environment to apply Bobath (...)”.
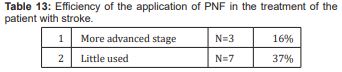
For one therapist: “(…) has better results in an acute phase than in a subacute or chronic phase (…)” Table 13.
For three interviewees: "(...) in terms of PNF, I use it in a more advanced phase (...).”
The choice or not of the application of the method, comes from the lack of scientific information about the method "(...) I do not use it much because at the time of graduation the PNF method was a bit lethargic or almost dead, there was not much research, validation of the method (...)". (N= 2).
The answers obtained "(...) I always see that it is more effective. The proprioceptive part, the touching of the patient, the correction, is effective (...)" (N=1), and "(...) obtained good results, although slower than in Bobath (...)" (N=1). From the analysis of several studies the PNF method is indeed effective, however it was not possible to obtain information about the time of evolution/response of the patient.
In general, the information obtained is in line with the literature, considering the assumptions and advantages of both methods. Bobath and PNF are two of the methods most used by occupational therapists, in the process of rehabilitation of patients with this pathology. It was possible to understand the need for specific training to deepen knowledge about the methods under study, since the lack of these trainings can influence the choice of methods to be used. The understanding of the concepts in their integration must be very well understood by those who propose to apply some methods when accompanying patients.29
For the application of the Bobath method, for example, an in-depth knowledge about the normal sequential development of motor behavior is necessary, since this relearning occurs through a hierarchy of nervous system functions (Cephalocaudal and Proximal-Distal)17 and results from the influence of the sensory stimuli provided, as well as feedback from the motor response produced by the patient throughout the rehabilitation process. Following the same line of thought, the intervention based on this methodology follows several steps, starting with positioning in a phase of sagging (after the occurrence of stroke), postural control and normalization of the tone (spasticity phase), and normalization of normal movement patterns.2 In the study The influence of NDT-Bobath and PNF methods on the field support and total path length measure foot pressure (COP) in patients after stroke, authors concluded for a greater
improvement, concerning the body balance, with the Bobath approach.30
The literature review suggests that the intervention of the occupational therapist should meet the needs of the patient and that this intervention should be evaluated and reevaluated at each stage of the rehabilitation process, to provide the appropriate treatment to each patient.1 PNF, otherwise, is based on neuromuscular facilitation techniques to provoke or facilitate motor responses and improve neuromuscular control and function.14 It can be used to develop muscle strength and endurance, promote joint stability, mobility, and neuromuscular control, and facilitate the coordination of movements,14 enabling the alteration or facilitation of motor patterns through sensory stimuli, namely proprioceptive, produces permanent effects on the CNS22. It is usually used at an early stage of the rehabilitation process, as preparation for the following phases.25
Verbal commands are necessary for the patient to obtain a better motor response, i.e., it is important that the patient understands what is proposed to him and the movement he is making, to make the intervention effective.19 The application of Bobath together with PNF revealed greater benefits when compared to its use in a unique way.13 Different studies show greater efficacy in rehabilitation treatment when it is carried out with the combination of others.31,32
In the randomized pilot study Effect of PNF and NDT Bobath Concepts in Improving Trunk Motor Control in Ischemic Stroke Patients, authors concluded for no significative difference between the two methods as results showed similar level of effectiveness on postural control. What concerns the phase of the rehabilitation process in which the methods should be applied, there is no consensus in the scientific literature that supports this information reported by the participants.
Despite the benefits of using the Bobath method, various studies state that the occupational therapists choose to use it, considering their personal preferences, ranging from the knowledge they have about their application, the context of professional performance, the time they must hold the sessions with patients or the materials at their disposal. From the literature review, PNF is a widely used method, as it contributes to the rehabilitation of the patient, increasing its level of functionality.19,20 However, it was not possible to prove at which stage of the rehabilitation process its application is most beneficial. The results corroborate the literature review, where the authors state that evidence is needed to prove that the exclusive application of the method is effective, because the methods are applied mostly in conjunction with other intervention techniques.19
Stroke is a very disabling disease that compromises the motor, cognitive and social functions of the individual, preventing him from performing the activities that are significant for himself. OT is an area of health that focuses on the recovery of functionality, promoting independence, well-being, and quality of life. This factor, on the other hand, compromises the evidence of efficacy of the methods, since the results obtained cannot be associated with only one technique, but with all those used throughout the rehabilitation process.
Regarding the patient's role in the rehabilitation process, it appears that both methods require active participation.
About the benefit of the applied method, the PNF is the one that is not so applied by therapists, as they do not recognize its effectiveness. As regards the Bobath method, it can be concluded that its use constitutes an added value. The use of this method allows the patient to recover its functionality with normal movement patterns, avoiding future complications at the musculoskeletal level that may result from the use of abnormal or inappropriate movement patterns.
Regarding the intervention phases in which the methods are applied, there is no concordance between the interviewees.
We consider the reduced number of interviewees to be a limitation of the study, as well as to their degree of experience. Most of the interviewees perform their functions in Hospital Units, mostly in inpatient services, which may affect the therapeutic approach and, consequently, the use of the methods under study, since in most cases there is a shortage of available materials and a reduced period to intervene with patients.
In general, the main results are in line with the literature, in what is considered about the assumptions and advantages of both methods. However, its efficacy as well as the stages of patient evolution was not evident, either in the literature or in the results obtained. Most interviewees use the Bobath method throughout the intervention process with greater emphasis at an early stage and use the PNF only at a more advanced stage of the rehabilitation process.
Thus, as mentioned in other studies, it is necessary to carry out new research projects on the methods under study in this population, which allow clarifying their effectiveness, the ideal duration of treatment, as well as the stage of evolution of the patient in which they should be applied. As a possible proposal for the continuity of the study, it is suggested that measurable and continuous records be made by occupational therapists to validate the effectiveness of their intervention, as well as the phases in which the application of the methods is best suited.
The researchers thank all the occupational therapists who kindly shared their time and knowledge, agreeing to participate in the study and making it possible to carry out this project, which aims to contribute to a greater knowledge about the intervention of OT with patients affected with stroke, using the intervention methods of Bobath and PNF.
None.
The authors declare no conflict of interest.
- 1. Pissaroli C, Almeida G, Luvizotto J, et al. Modelos de reabilitação fisioterápica em pacientes adultos com sequelas de AVC isquémico. Revista Neurociências. 2012;20(1):128–137.
- 2. Kuklinska P, Gackowska M. Rehabilitation after ischemic stroke in the elderly. Journal of Education, Health and Sport. 2020; 10(8):340–345.
- 3. Lako A, Cani E, Bara R, et al. Cerebral stroke, hemiplegy, recovery and rehabilitation during the period 2004-2014, QSUT. International Journal of Scientific and Research Publications. 2015;5(12):391–393.
- 4. Schneider apud Ribeiro MBS, Oliveira LR. Terapia ocupacional e saúde mental: construindo lugares de inclusão. Interface. 2005; 9(17):425–431.
- 5. Ferreira T, Oliver F. Terapia ocupacional em disfunção física: discutindo a produção bibliográfica brasileira no período de 1999 a 2005. Revista de Terapia Ocupacional da Universidade de São Paulo. 2006;17:108–114.
- 6. Thame A, Pinho P, Reys B. et al. A reabilitação funcional o membro superior em pacientes espásticos, pós Acidente Vascular Cerebral (AVC). Neurociências. 2010;18(2):179–185.
- 7. World federation of occupational therapists – WFOT, About occupational therapy. Recuperado de. 2012.
- 8. Shin CG, Toldrá RC. Terapia ocupacional e acidente vascular cerebral: revisão integrativa da literatura. Cadernos de Terapia Ocupacional. 2015;843–854.
- 9. Jarus T. Motor learning and occupational therapy: the organization of practice. American Journal of Occupational Therapy.1994;810.
- 10. Paci M. Physiotherapy based on the Bobath Concept for adults with post-stroke hemiplegia: A review of effectiveness studies. Pubmed. 2003;35:2–7.
- 11. Francisco S. Modelos de intervenção em fisioterapia nos pacientes com espasticidade pós AVC: Revisão da Literatura. (Tese de Mestrado). Instituto Politécnica de Lisboa, Escola Superior de Tecnologia de Saúde de Lisboa, Lisboa. 2016.
- 12. Nadu T. Effectiveness of Bobath approach on trunk balance in patients with stroke (Master’ thesis). College of Physiotherapy, Coimbatore. 2019.
- 13. Souza W, Conforto A, André C. Terapia de restrição e indução do movimento em pacientes pós-AVC. Fisioterapia Brasil. 2007; 8:64–68.
- 14. Nadu T. A comparative study on the effectiveness of Bobath approach and Proprioceptive Neuromuscular Facilitation Technique in gait training and balance among chronic stroke patients. (Master’ thesis). College of Physiotherapy, Coimbatore. 2016.
- 15. Soderback I. International handbook of occupational therapy interventions. Suécia: Springer. 2009.
- 16. Silva LB, Pinto SL, Fabrin SC, et al. Revisão integrativa quanto aos efeitos do conceito de Bobath na recuperação funcional de pacientes com a doença cérebro vasculares. Brasil: Centro Universitário UNIFAFIBE. 2022.
- 17. Flanagan EM. Methods for facilitation and inhibition of motor activity. American Journal of Physical Medicine. 1967;46(1):1006–1011.
- 18. Dietrich A, Mokan PP, Fuhrmann GW, et al. Tratamento fisioterapêutico de pacientes com AVC – revisão da literatura. Brasil: Salºao do conhecimento INIJÚI. 2016.
- 19. Mesquita M, Mejia D. Efeitos da facilitação neuromuscular propriocetiva (FNP) na melhoria global do paciente acometido por acidente vascular cerebral (AVC). (Pós-graduação). Faculdade Ávila.
- 20. Marques P. Os benefícios do método PNF nas disfunções neurológicas. 2017.
- 21. Silva A, Garfenghi G. eficácia da técnica de facilitação neuromuscular propriocetiva (FNP) no tratamento da hemiparesia em pacientes com Acidente Vascular Encefálico Isquémico. 2019.
- 22. Wilma Costa Souza.Terapia de restrição e indução do movimento em pacientes pós-AVC. Fisioterapia Brasil. 2007:(8);64– 68.
- 23. Pin A, Filho M. Facilitação neuromuscular proprioceptiva nas alterações musculares. Novas Edições Acadêmicas. 2016.
- 24. Barreto E. Aplicação da facilitação neuromuscular propriocetiva em pacientes após acidente vascular encefálico. 2019.
- 25. Fortin M, Catê J, Filion F. Fundamentos e etapas do processo de investigação. Loures: LUSODIDATA. 2006.
- 26. Guazi T. Diretrizes para o uso de entrevistas semiestruturadas em investigações científicas. Revista Educação, Pesquisa e Inclusão. 2021;2:1–20.
- 27. Fontanella BJ, Campos CJ, Turato ER. Coleta de dados na pesquisa clínico-qualitativa: uso de entrevistas não-dirigidas de questões abertas por profissionais de saúde. Revista Latino-am Enfermagem. 2006;1-10.
- 28. Mackey Alison; GASS, Susan. Second language research: methodology and design. New Jersey: Lawrence Erlbaum Associates, 2005:405.
- 29. Krukowska J, Bugajsky M, Sienkie W, et al. The Influence of NDT_Bobath and PNF Methods on the field support and total path length measure foot pressure (COP) in patients after stroke. Neurol Neurochir Pol. 2016;50(6):449–454.
- 30. Kuciel M, Rutkowsky S, Szary P, et al. Effect of PNF and NDT Bobath Concepts in Improving Trunk Motor Control in Ischemic Stroke Patientes – a Randomized Pilot Study. Medical Rehabilitation / Rehabilitacja Medyczna (Med Rehabil). 2021;25(2):4–8.
- 31. Claro IG, Leiva MI. Aplicación del método Bobath en pacientes que han sufrido un accidente cerebrovascular. TOG (A Coruña). 2015;1–18.
- 32. Costa J, Perera A, Cordero J, et al. Resultados de la aplicación de un programa de rehabilitación física en pacientes con síndrome hemiplégico por enfermedad cerebrovascular. Revista Colombiana de Medicina Física y Rehabilitación. 2011;21(2):68–75.

