Angiomyomatous hamartoma of head and neck region is very are disease, of unknown etiology and more often than not it can be misdiagnosed preoperatively.
Materials and Methods: In a study we present a case of angiomyomatous hamartoma in the carotid triangle, a site where a tumor has an invasion to external carotid artery, treatment carried out by surgical excision, after histological examination, the final diagnosis was made. The patient was under observation for 3 years, there were no relapses.
Conclusion: The diagnosis of angiomyomatous hamartoma is based on histologic examination. Although this entity is rare, we believe that head and neck surgeons should include it in the differential diagnosis of head and neck masses.
Keywords: Angiomyomatous hamartomas, Head and neck region carotid artery, Chemodectomy
Ahamartoma (from Greek hamartia, meaning “fault, defect,” and-oma, denoting a tumor or neoplasm) is a focal proliferation of cells and tissues typically found in the organ from which they arise. In spite of being characterized by the presence of mature elements, the architecture of the organ is not preserved. Eugen Albrecht is credited with first using the term hamartoma in 1904. Albrecht described hamartomas as tumour-like formations in which there is an abnormal mixture of normal components of the organ in which they occur either by amount, structure and degree of maturity or all three together.1,2 The line of demarcation between hamartomas and benign neoplasms is often unclear, since both lesions can be clonal. A hamartoma, however, contrary to a neoplasm, shows a self-limited growth. Hamartomas are composed of a mix of mesenchymal tissues and can be classified into different types according to the predominant tissue composing them: bone-forming, cartilage-forming, fibre-forming and non-matrix-forming hamartomas.3 They can arise in virtually all organ systems, either sporadically or in association with syndromic entities, some of which have a well-known genetic basis. One of the types of hamartomas is angiomyomatous hamartoma, which is one of the rare causes of a symptomatic lymphadenopathy with unknown etiology: commonly affecting the inguinal and femoral lymph nodes. It is characterized by replacement of lymphoid follicles by haphazardly arranged combination of smooth muscle bundles, fibrous tissue and thick-walled blood vessels.4 Only few cases in the head and neck region have been documented in the literature.5,6 It should be borne in mind that hamartoma is one of the differential diagnoses of unilateral, painless, progressive vascular vascular edema of the cheek that does not respond to propranolol. Hemangioma should be ruled out be for hamartoma is diagnosed, which is rare. Treatment can be reached only by surgical excision. Diagnosis is confirmed on histopathology. We present a case of angiomyomatous hamartoma in the carotid triangle, a site where a tumor has an invasion to external carotid artery.
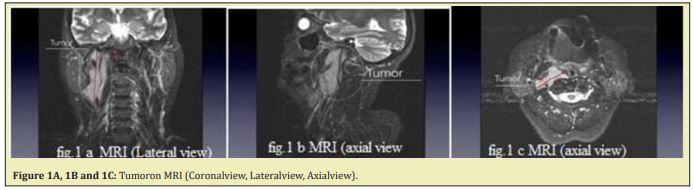
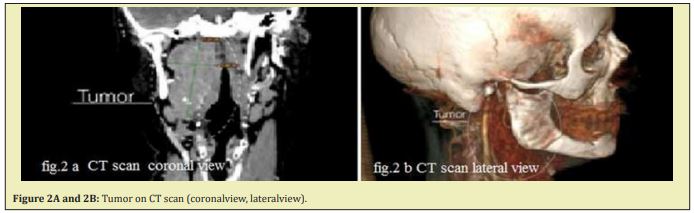
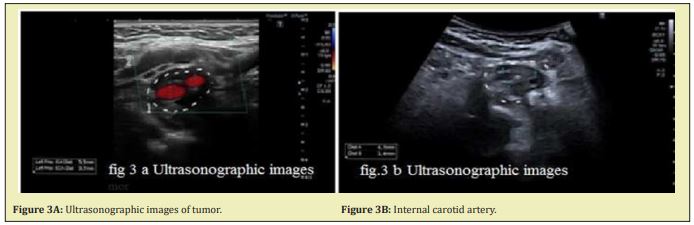
A 63 years-old woman admitted to Oral and Maxillofacial surgery department with complaints of painless, slow growing mass that had been present for 1.5 year in right side of the neck. She reported that the mass had grown significantly over the previous year. On physical examination, a 4cm diameter elastic carotid triangle mass was palpated. No skin involvement or fluctuation was noted. No lymph nodes were palpated. MRI Figure 1A, 1B, and 1C and contrast enhanced CT scan Figure 2A and 2B. Revealed hyper enhanced mass measuring 7,29cmx3,89cm From right carotid bifurcation until the skull base. Ultrasonography demonstrated a hypoechoic, non homogeneous mass 4.5x1.2x1.2cm-size that involved most of the external carotid artery in bifurcation without invasion of surrounding tissue Figure 3A and 3B. On Fine-needle aspiration cytology diagnosis of carotid body tumor was made. The mass was diagnosed as an external carotid paraganglioma.
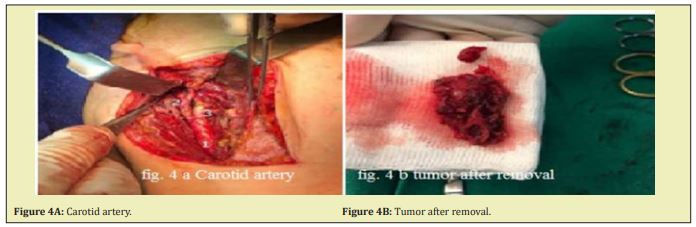
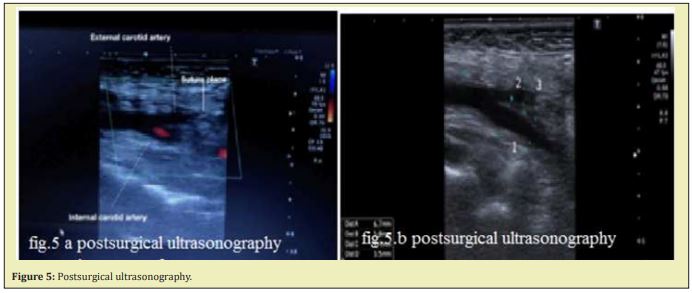
After appropriate preoperative evaluation patient was hospitalized and under general endotracheal anaesthesia it was performed an vertical incision on the anterior border of SCM muscle started from retromandibular region and continued until the level of hyoid great wing 8cm. Incision continued until endocervical fascia and carotid artery was identified and tight with suture above the thyroid superior artery and complete excision of tumor was performed and pathohistological examen accomplished Figure 4A and 4B. Wound was closed with three layers endocervical fascia, platysma and skin. Patient took intra venous cephalosporin1g for 5 days and anti-inflammatory drugs. Postoperative ultrasonography was per formed Figure 5A and 5B. Histopathology revealed a firm encapsulated soft tissue mass of size 4.6x1.4x1.2cm and the conclusion was cervical angiomyomatous hamartoma Figure 6A, 6B, and 5C. The patient was discharged after 7 days of hospital stay free of symptoms and in good general condition.
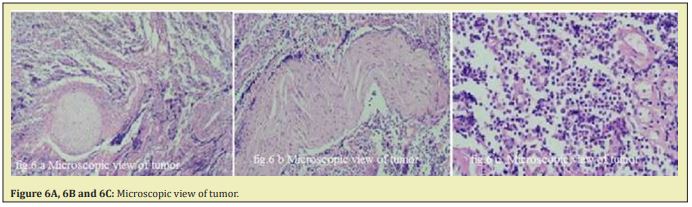
Hamartomas are classified according to their predominant elements into two types as epithelial (seromucinous, respiratory or salivary) and mesenchymal (angiomatous, chondroid, lipomatous or neurogenic).1,4 Histologically, hamartoma must be differentiated from other developmental tumors like teratoma and dermoid.6 Hamartomas are most commonly derived from mesoderm whereas dermoid is derived from ectoderm & mesoderm and teratoma from all three germinal layers. Hamartomas may occur in any organ because they represent a focal over growth of mature normal cells and tissues at sites of identical cellular composition. They may arise from any germ layers. They do not metastasize in their original description of angiomyomatous hamartomas, Chanetal noted that they are characterized by a prolife ration of thick-walled hilar blood vessels that extend in to the nodal parenchyma.7 In a study conducted to examine the morphological and clinical findings of various primary vascular tumors of lymph nodes other than Kaposi's sarcoma, Chanetal. Used the term “angiomyomatous hamartoma” to describe a characteristic clinical and pathological lesion arising in the lymph nodes. Although the selesions have been described as occurring throughout the body, they are rare in the head and neck region. While Fine et al8 reported 60 cases of laryngeal hamartoma, there are only isolated reports of these lesions in other head and neck sites, such as the ethmoid sinus,5 hard palate,9 nasopharynx,10 neck5,11 and parotid gland.5,12 For diagnosis the Ultrasonography(US) is an accurate, cost-effective, non-invasive preoperative analysis, usually sufficient to make correct preoperative diagnoses, even if the accuracy of this imaging method may have limitations, because of the variability of the sono graphic appearances.13,14
Microscopically these lesions show complete or partial replacement of the lymph nodal parenchyma with prolife ration of the blood vessels, smooth muscle cells and connective tissue stroma.15 Surgical resection is the treatment of choice and till date no recurrence has been reported. Nevertheless, there are chances for recurrences, especially when excised incompletely. There are no other documented treatment options for hamartoma anda close clinical follow up is all that is required. The clinical course of hamartoma is mostly benign, does not tend to spontaneous regression, and the treatment of choice is complete surgical removal.16 However, there is a chance of relapse, especially if the removal is incomplete. In study we present a case of angiomyomatous hamartoma in the carotid triangle, a site where a tumor has an in vision to external carotid artery, treatment carried outby surgical excision, after histological examination, the final diagnosis was made. The patient was under observation for 3 years, there were no relapses.
The diagnosis of angiomyomatous hamartoma is based on histologic examination. Once the diagnosis has been established, complete excision of the lesion is the treatment of choice. Although this entity is rare, we believe that head and neck surgeons should include it in the differential diagnosis of head and neck masses.
None.
Non funding
The author declares that he has no conflict of interest and there was no external source of funding for the present study. None of the authors have any relevant financial relationship(s) with a commercial interest.
- 1. Albrecht E Über. Hamartoma. Verh Dtsch Ges Pathol. 1904;7:153–157.
- 2. Ober WB. Selected items from the history of pathology: Eugen Albrecht, MD (1872-1908): hamartoma and choristoma. Am J Pathol. 1978;91:606.
- 3. Owens D, Alderson D, Garrido C. Nasopharyngeal hamartoma: importance of routine complete nasal examination. J Laryngol Otol. 2004;118(7):558–560.
- 4. Ghosh P, Saha K, Gosh AK. Vascular transformation of bilateral cervical lymph node sinuses: a rare entity masquerading as tumor recurrence. J Maxillofacial Oral Surgery. 2015;14:397–400.
- 5. Samuel J, Fernandes CC. Hamartomas of the head and neck. Areportof4 cases. SAfr Med J. 1985;68(4):265–267.
- 6. Windfuhr JP. Laryngealhamartoma. Acta Otolaryngol. 2004;124(3):301–308.
- 7. Chan JK, Frizzera G, Fletcher CD. Primary vascular tumors of lymph nodes other than Kaposi's sarcoma. Analysis of 39 cases and delineation of two new entities. Am J Surg Pathol. 1992;16(4):335–350.
- 8. Fine ED, Dahmas B, Arnold JE. Laryngeal hamartoma: a rare congenital abnormality. Ann Otol Rhinol Laryngol. 1995;104(2):87–89.
- 9. Harada H, Morimatsu M, Kusukawa J, et al. A hamartoma-like mass on the palate? A possible discussion regarding the components of a pigmented naevus and hyperplastic salivary gland. J Laryngol Otol. 1997;111(3):296–299.
- 10. Majumder NK, Venkatararnaniah NK, Gupta KR, et al. Hamartoma of nasopharynx. J Laryngol Otol. 1977;91(8):723–727.
- 11. Laeng RH, Hotz MA, Borisch B. Angiomyomatous hamartoma of a cervical lymph node combined with haemangiomatoids and vascular transformation of sinuses. Histopathology. 996;29(1):80–84.
- 12. Tsuda H, Morinaga S, Mukai Ketal. Hamartoma of the parotid gland: a case report with immunohistochemical and electron microscopic study. Virchows Arch A Pathol Anat Histopathol. 1987;411(5):473–478.
- 13. Sidell DR, Shapiro NL. Diagnostic Accuracy of Ultrasonography for Midline Neck Masses in Children. Otolaryngol Head Neck Surg. 2011;144(3):431–434.
- 14. Friedman ER, John SD. Imaging of pediatric neck masses. Radiol Clin North Am. 2011;49(4):617–632.
- 15. Mauro CS, Mc Gough RL, Rao UN. Angiomyomatous hamartoma of a popliteal lymph node: an unusual cause of posterior knee pain. Ann Diagn Pathol. 2008;12:372–374.
- 16. Jain RK. Hamartoma of the head and neck. Indian J Otolaryngol Head Neck Surg. 1999;51(4):76–78.

