Isolated spontaneous coronary intramural hematoma is characterized by a hemorrhage limited to the media–adventitial layers, causing subsequent hematoma formation without visible intimal flaps. Spontaneous isolated intramural hematoma may occur in the absence of associated intimal dissection. It is an infrequent and serious coronary vessel wall pathology with poorly understood underlying pathogenic mechanisms. Affected individuals may present with a broad spectrum of symptoms ranging from acute coronary syndromes (ACS) to cardiogenic shock or even sudden cardiac death. The disease entity causes challenges in terms of both diagnostic and treatment strategy. We report a case of intramural coronary hematoma in a patient presenting with non ST-segment elevation myocardial infarction.1
Keywords: Coronary hematoma, Coronary lesions, Coronary blood
Spontaneous coronary intramural hematoma in major epicardial coronary vessels is a rare cause of chest pain. The hematoma formation is limited to the media–adventitial layers, and no flaps are visible when assessed with tomographic techniques.1,2 This serious condition usually presents as acute coronary syndrome (ACS) but symptoms may range from chest pain to cardiogenic shock or sudden death,1,2 depending on hematoma location, number of affected vessels, lumen compromise and restriction of coronary blood flow. It is more frequent in young women, particularly in the peri and post- partum period and with oral contraceptive use, and in young and middle-aged patients without obvious cardiovascular risk factors.3,4 Management strategies may range from conservative medical treatment to percutaneous or surgical interventions depending upon the anatomy, extent of the hematoma and the clinical circumstances.5,6 We report a case of intramural coronary hematoma in a patient presenting with non ST- segment elevation myocardial infarction.
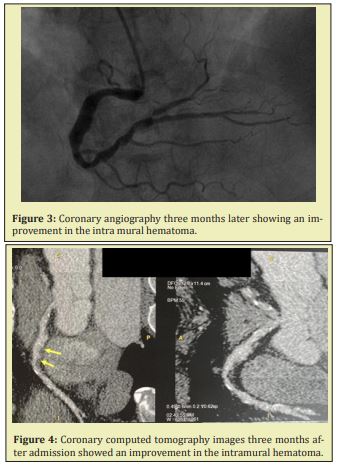
A 64 -year old female was admitted due to sudden onset of chest pain. Cardiovascular risk factors included hypertension. The ECG showed inverted T waves in inferior and low lateral leads. Troponin-I was elevated (8,52ng/ml). The echocardiogram showed normal wall motions and preserved EF. Coronary angiography revealed an ectasic right coronary artery, where we detected a large intra mural hematoma starting from mid segment of the RCA. Unfortunately, neather the IVUS or the OCT is available in our hospital. We performed a coronary computed tomography for a more detailed evaluation of the morphological features of the vessel wall. We therefore decided to continue conservative treatment and intensified the medical therapy. She was discharged after one week in a stable clinical condition on aspirin and clopidogrel. A repeat angiogram three months later showed an improvement in the intra mural hematoma and remains free of cardiac events at 12 months.

Diagnosis of intramural hematoma should be considered in any middle-aged female with a paucity of risk factors for atherosclerosis, presenting with sudden onset of ischemic chest pain. Women appear to be primarily afflicted and the incidence is increased in the peripartum and postpartum periods, probably due to hormonal factors. Other known risk factors are vasculitis, hypertension and illegal drugs. The exact pathophysiology is unclear, but it is thought to be due to disruption of the vasa vasorum leading to hematoma formation in the media of the arterial wall.7
Coronary angiography is not sufficient to identify the cause of acute coronary syndrome. Intracoronary imaging techniques such as IVUS and OCT can provide much more detailed information about the morphologic features of the coronary artery, including entry tear, flap, and associated thrombus.8
The proper management of coronary intramural hematomas is currently unestablished. Treatment is usually based on the presentation and presence of ongoing ischemia. Some cases have been managed with coronary bypass, others with intracoronary stenting9 or conservative medical treatment. In cases treated by stenting, there have been reports of late stent malapposition and a risk factor for stent thrombosis thought to be due to resorption of the intramural hematoma over time.10
Information regarding the long-term prognosis after isolated spontaneous coronary hematomas is extremely sparse due to the limited number of cases reported. PCI treatment has been documented with a high rate of complication and procedural failure. In spite of better long-term survival in comparison with typical ACS-patients, rates of later major adverse events have been found to be high.11
A spontaneous intramural hematoma is one of the possible causes of acute coronary syndrome. Intracoronary imaging techniques such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) can provide detailed morphological information on coronary lesions, which is useful for an accurate diagnosis and the selection of an appropriate treatment strategy.
None.
None.
Author declares that there is no conflict of interest.
- 1. Hanratty CG, McKeown PP, O`Keeffe DB. Coronary stenting in the setting of sponta- neous coronary artery dissection. Int J Cardiol. 1998;67:197–199.
- 2. DeMaio Jr SJ, Kinsella SH, Silverman ME. Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol. 1989;64:471–474.
- 3. Raja Y, Trevelyan J, Doshi SN. Intramural hematoma presenting as acute coronary syndrome: the importance of intravascular ultrasound. Cardiol J. 2012;19:323–325.
- 4. Ikegami R, Tsuchida K, Oda H. Acute myocardial infarction caused by spontaneous coronary intramural hematoma. J Invasive Cardiol. 2012;24:692–693.
- 5. Poon K, Incani A, Small A, et al. Drug eluting stents trapping intramural hematoma in spontaneous coronary artery dissection and healing pattern at six months: optical coherence tomography findings. Cardiovasc Revasc Med. 2013;14:183–186.
- 6. Gowda RM, Sacchi TJ, Khan IA. Clinical perspectives of the primary spontaneous cor- onary artery dissection. Int J Cardiol. 2005;105:334–336.
- 7. Raja Y, Trevelyan J, Doshi SN. Intramural hemotoma presenting as acute coronary syndrome: the importance of intravascular ultrasound. Cardiol J. 2012;19(3):323–325.
- 8. Alfonso F, Paulo M, Gonzalo N, et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. J Am Coll Cardiol. 2012;59:1073–1079.
- 9. Auer J, Punzengruber C, Berent R et al. Spontaneous coronary artery dissection involving the left main stem: Assessment by intravascular ultrasound. Heart. 2004;90:e39.
- 10. Sanchez Recalde A, Moreno R, Jimenez Valero S. Stenting of spontaneous intramural coronary haematoma: Long-term consequences. Eur Heart J. 2008;29:1593.
- 11. Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126:579–588.

