Aim: To evaluate the knowledge, attitude and practice about diabetic retinopathy among diabetic patients, attending the endocrinology department of Nampula Central Hospital in Mozambique.
Materials and Methods: A descriptive cross-sectional study was conducted at Endocrinology Department of Nampula Central Hospital in Mozambique. Patients' knowledge, attitude and practice were assessed using a 90-point semi-structured questionnaire. Patients were classified into different categories according to their knowledge, attitude and practice. Data analysis was performed with the aid of SPSS version 20, where frequency distribution and measures of central tendency (mean, median and standard deviation) were used to summarize the descriptive part of the study. The median of Likert scale was calculated and used to identify the majority opinion for questions related to Diabetic retinopathy. Participants were included in the study as part of the sample after signing informed consent.
Results: A sample of 305 participants was studied, where 163(53.4%) were male and 142(46.6%) were female; the mean age of the participants was 52.08(±13.04) years. The mean duration of diabetes was 7.2(±6.3) years. The most prevalent treatment was the combination of diet with medication represented by 51.8%. The participants had an average score of 3.98 in the knowledge section and a satisfaction level of 58.0%. The average score in the attitude was 2.92, being negative in 51.5%, and about practice they scored in average 3.49, being positive in 51.5% of the participants.
Conclusion: Study participants have satisfactory knowledge and favorable practices regarding diabetic retinopathy, but the majority's attitude is negative.
Keywords: Knowledge, Attitude, Practice, Diabetic retinopathy, Endocrinology
Diabetes mellitus is a group of physiological disorders characterized by hyperglycemia resulting directly from insulin resistance, inadequate insulin secretion or excessive glucagon secretion.1,2 The global prevalence of diabetes mellitus has increased from 4.7% in 1980 to 8.5% in 2014, increasing the number of adults with diabetes to a staggering 422 million worldwide, according to the World Health Organization and it is estimated that 642 million people are expected to be diabetic by 2040.3,4
Diabetic retinopathy (DR) is a microangiopathy of the retina. It involves changes in the vascular wall and in the rheological properties of blood.5 Visual impairment as a result of diabetic retinopathy has a significant negative impact on a patient's quality of life and their ability to successfully manage the disease.6,7
The proportion of global blindness due to DR has increased from 2.1% in 1990 to 2.6% in 2010.8 Globally DR accounts for 5% of all blindness, affecting 2 million people, and is the leading cause of blindness in people aged between 15 and 64 years in industrialized countries. It has been estimated that DR blindness could be reduced by up to 90% if agreed treatment protocols and standardized care for diabetics were implemented.9-11 The prevalence of DR among patients with diabetes is 34.6% worldwide. Early detection depends on a regular eye exam involving assessment of visual acuity and ophthalmoscopy through dilated pupils by experienced personnel.12,13
It is necessary to identify the risk factors that affect the occurrence of DR for the development of clinical management strategies to slow the progression of the disease and prevent visual loss.14 Some factors related to the diabetic state are postulated to play a causal role in this disorder.15 Prevention of blindness from diabetic retinopathy requires effective screening strategies, for which ophthalmologists need to know the magnitude of the burden and pertinent risk factors in their geographic location.16
Early detection, implementation of effective screening programs, and efforts to control risk factors for DR are crucial to delay onset and slow disease progression and also there are highly effective and low-cost treatments for RD. Up to 98% of blindness can be prevented with laser treatment and/or vitreous surgery.17,18
Although early detection of diabetic retinopathy is critical to preventing vision loss, many patients are not adequately evaluated. Using a multidisciplinary approach, primary care physicians and ophthalmologists should follow evidence-based recommendations for screening and monitoring diabetic patients as they work to improve glycemic index and blood pressure.19 Despite the growing concerns about the emergence of DM as a major public health problem, there is still much to be understood about the epidemiology of DR.20
Therefore, strategies must be implemented to detect DR in the early stages and manage them based on international standards. Early detection and treatment will reduce visual morbidity associated with diabetes complications. Diabetic patients must be considered as important stakeholders in this process.21
This was a cross‑sectional study to assess the knowledge, attitude and practice related to diabetic eye disease among patients with diabetes. The study was conducted among diabetic patients attending the endocrinology department of Nampula Central Hospital in Mozambique. The sample size was calculated based on the unknown prevalence for KAP (50%), with z=1.96, for a population of 1454 diabetic patients attending the endocrinology department at Nampula Central Hospital in Mozambique, considering a significance level of 5% and 95% confidence interval. The final estimated sample size was 305.
Previous to the data collection, the protocol was submitted and approved by the Lúrio University Institutional Ethical Review Board. This study is in accordance with the tenets of the Declaration of Helsinki (2013). All patients with confirmed diagnose of DM attending the endocrinology department during the period of February to June 2022 were invited to participate in this study.
All of those who accepted, provided signed informed consent and face-to-face interviews were held to gather responses to a validated 18‑item questionnaire developed to measure knowledge (9items), attitude (6 items), and practice (3 items) about diabetic eye complications and eye care. Additional 4-items questions were performed to access demographic features of study participants (age, gender, duration of diabetes and treatment).
The questionnaire was framed in English based in the validated information available in the literature from previous published studies in the topic and translated to Portuguese by a Portuguese lecturer at Lúrio University. Therefore the back translation was performed by an English Lecturer to ensure language equivalence between the English and Portuguese versions of the scale.
Three optometrists provided opinions about meaning and content sufficiency. A pilot study Performed with 72 patients of a similar population was then conducted in January 2022 to determine whether there were any unclear questions in the scale. The data from the pilot study were not included in the final data analysis.
Responses to each item were measured on a 5‑point Likert scale (ranging from “Fully disagree-1” to “Fully agree-5”). Each item was scored out of a maximum of 5 points and minimum of 1 point.
The Statistical Package for the Social Sciences (SPSS) version 20.0 was used for data entry and analysis. Data were described using mean, median and standard deviation (SD).Frequencies and percentages were calculated and presented to describe the findings.
Knowledge about DR was categorized as Satisfactory for individuals where the average score was equal or superior to the mean value of 3.98 and dissatisfactory if the average score was less than the mean value. The Attitude was categorized as Positive if the average score was equal or superior to the mean value of 2.92 and Negative if it was lower. The Practice was named Favorable if the average score was equal or superior to the mean value of 3.49 and Unfavorable if it was lower than the mean.
From 305 respondents, 142(46.6%) participants were female and 163(53.4%) were male. The mean age was 52.08(±13.04). According to the age distribution, 6(1.96%) participants were aged between [14-18] years, 5 (1.64%) participants were [19-23] years, 3(0.98%) participants were [24-28] years old, 7(2.29%) participants were [29-33] years old, 18(5.9%) participants were [34-38] years, 34(11.1%) were [39-43] years and 232(76.0%), were over 43 years old.
The mean duration of diabetes diagnosis was 7.2(±6.3) years. 68(22.2%) out of 305 participants reported to be under treatment of diabetes for more than 10 years, 84(27.5%) participants reported [6-10] years and 158(50.1%) participants reported [1-6] years. As for the type of treatment, 11(3.6%) participants mentioned they are under medication only, 136(44.6%) mentioned they follow a recommended balanced diet only and 158(51.8%) are under the combination of both methods (recommended balanced diet and medication). The information regarding demographic features of the study population is summarized in Table 1.
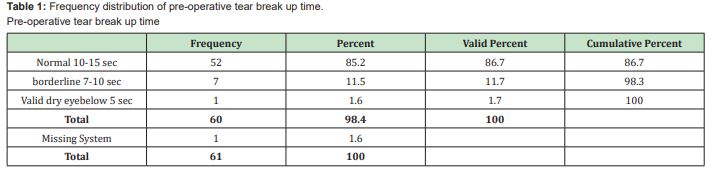
Table 2 summarizes the information regarding the distribution of responses according to the 5-point Likert scale related to knowledge, attitude and practice of diabetic retinopathy.
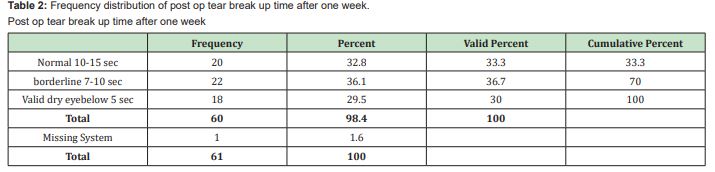
About the knowledge related questions, 240(78.7%) strongly agreed that diabetes can damage the eyes and vision while 215(70.5%) participants strongly agreed that receiving treatment on time can prevent or delay eye damage due to diabetes, 201(65.9%) participants strongly agreed that the risk of eye complications increase with poor control of diabetes, 200(65.6%) participants strongly agreed that eye treatments are successful if blood sugar is controlled, 149(48.9%) strongly agreed that Children who have diabetes are also at risk of developing eye complications, 120(39.3%) strongly agreed that the ophthalmologist can find out the effects of diabetes on the eye with the use of special equipment. When questioned if in diabetes, the eyes can be affected one at a time; if diabetes-related eye complications are treated well, the eye will not need treatment again and if eye treatments for people with diabetes are painful, 123(40.3%);102(33.4%) and 165(54.0%) participants are not sure.
Participants' attitude was assessed based in 6 questions. 166(54.4%) participants equal strongly agreed that they don't need regular (annual) eye exams even when the blood sugar level is under control and that only physicians should provide information about eye problems due to diabetes while 130(42.6%) mentioned that they control the blood sugar even when receiving treatments related to diabetes eye complications, 126(41.3%) strongly agreed that they don't need regular eye exams when the eyesight is good, 182(59.7%) strongly disagreed that it is a waste of time and money for people with diabetes to go for an eye exam if their eyesight is normal and 178(58.4%) strongly disagreed that they don't need to worry about blood sugar control when having eyes treatment.
Practice about DR was evaluated based in 3 questions. 214(70.1%) strongly agreed that If suddenly the vision gets worse and they can't see well, they have to go for an eye exam, 89(29.1%) strongly agreed that they go for a regular (annual) eye check-up appointment because of diabetes while 123(40.3%) strongly disagreed they have received advice on the prevention and treatment of diabetic eye complications from an ophthalmology team.
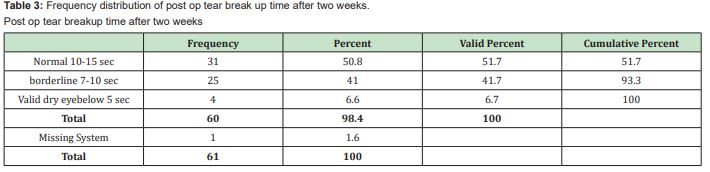
The median score of questions related to knowledge was 3.98; where 128(42.0%) participants have dissatisfactory knowledge about diabetic retinopathy and 177(58.0%) have satisfactory knowledge. Nevertheless, the median score for attitude related questions were 2.92, where 148(48.5%) participants demonstrated positive attitude and 157(51.5%) a negative attitude. Practice related questions about diabetic retinopathy had a median score of 3.49, where 148(48.5%) participants, have unfavorable practice, and 157(51.5%) have favorable practice. The Whole information about the classification of knowledge, attitude and practice of study participants in related to DR is summarized in Table 3.
This is the first study carried out in Mozambique to assess the knowledge, attitude and practice of diabetic patients about diabetic retinopathy.
The mortality, morbidity and cost-related complications of diabetes are increasing worldwide and are a persistent global public health problem. Diabetic retinopathy (DR) is considered the cause of blindness in 1.8 million of 37 million cases (4.5%) worldwide.22
In the present study, men were more representative with 53.4%. This result is lower than the result found in the study carried out in Saudi Arabia, but it is superior to the results found in China and Nigeria.23-25 The discrepancy in results may be associated with differences in the socio demographic characteristics of the population in each study.
The results of the present study indicate a satisfactory level of knowledge about diabetic retinopathy in 58.0% of the participants. This result is higher than the results of studies carried in Saudi Arabia, Goa, Sudan and Brazil, but lower than the results of studies carried out in Kenya and in Oman.26-31
The attitude towards screening and treatment of diabetic retinopathy in our study was positive in 48.5% of patients. It is higher than the study carried out in India but lower than the results found in other study in southern India.32,33
Recommendations for annual screening for diabetic retinopathy without health education may result in increased adherence to screening in the short term. Furthermore, if there is no feedback on the status of diabetic retinopathy by healthcare professionals, negative attitudes may develop among diabetic patients against regular screening for diabetic retinopathy.34
The annual screening practice for diabetic retinopathy was 51.5% in our study. This result is higher than the one found in the study carried out in Bangladesh, however lower than the result found in Saudi Arabia.35,36
The study demonstrated the existence of a satisfactory level of knowledge regarding diabetic retinopathy, in addition to favorable practices among patients with diabetes who attended the endocrinology department of Nampula Central Hospital in Mozambique, but patient’s attitude is mostly negative.
Improved availability of resources by healthcare professionals may not produce favorable results if patients do not understand the importance of early detection.
From this study, there is evidence of the need to reinforce dissemination and education activities with the aim of improving the situation around knowledge, attitude and practices on diabetic retinopathy.
Authors would like to address their gratitude to all the participants who accepted to make part of the study. Our gratitude is also addressed to the department of endocrinology of Nampula Central Hospital in Mozambique.
None.
The authors do not refer any type of interest.
- 1. Stabley JN, Towler DA. Arterial calcification in diabetes mellitus: Preclinical models and translational implications. Arterioscler Thromb Vasc Biol. 2017;37(2):205–17.
- 2. Blair M. Diabetes Mellitus Review. Urol Nurs. 2016;36(1):27–36.
- 3. Kanter JE, Bornfeldt KE. Impact of diabetes mellitus. Arterioscler Thromb Vasc Biol. 2016;36(6):1049–1053.
- 4. Tóth G, Szabó D, Sándor GL, et al. Diabetes and diabetic retinopathy in people aged 50 years and older in Hungary. Br J Ophthalmol. 2017;101(7):965–969.
- 5. Ulbig MW, Kollias AN. Diabetische Retinopathie: Frühzeitige Diagnostik und Effiziente Therapie. DtschArztebl. 2010;107(5):75–84.
- 6. Hendrick AM, Gibson M V, Kulshreshtha A. Diabetic Retinopathy. Prim Care Clin Off Pract. 2015;42(3):451–464.
- 7. Simó-Servat O, Hernández C, Simó R. Diabetic Retinopathy in the Context of Patients with Diabetes. Ophthalmic Res. 2019; 62(4):211–217.
- 8. Urthy GVS, Das T. Diabetic care initiatives to prevent blindness from diabetic retinopathy in India. Indian J Ophthalmol. 2016;64(1):50–54.
- 9. Prevention of blindness from diabetes mellitus. J Glob Health. 2006;p. 9–11.
- 10. Yau JWY, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–564.
- 11. Kyari F, Tafida A, Sivasubramaniam S, et al. Prevalence and risk factors for diabetes and diabetic retinopathy: Results from the Nigeria national blindness and visual impairment survey. BMC Public Health. 2014;14(1):1–12.
- 12. Thomas RL, Halim S, Gurudas S, et al. IDF Diabetes Atlas: A review of studies utilising retinal photography on the global prevalence of diabetes related retinopathy between 2015 and 2018. Diabetes Res Clin Pract. 2019;157:107840.
- 13. Ngah NF, Muhamad NA, Asnir ZZ, et al. Descriptive assessment on diabetic retinopathy screening in an awareness programme in Malaysia. Int J Ophthalmol. 2020;13(11):1808–1813.
- 14. Sun Q. Assessment for the Correlation Between Diabetic Retinopathy and Metabolic Syndrome : A Cross-Sectional Study. Diabetes Metab Syndr Obes. 2021;14:1773–1781.
- 15. Gao L, Xin Z, Yuan MX, et al. High prevalence of diabetic retinopathy in diabetic patients concomitant with metabolic syndrome. PLoS One. 2016;11(1):1–10.
- 16. Raman R, Gella L, Srinivasan S. Diabetic retinopathy: An epidemic at home and around the world. Indian J Ophthalmol. 2016;64(1):69–75.
- 17. Alhejji AE, Alsultan MA, Alshareet MA, et al. Knowledge, attitudes, and practices regarding diabetic retinopathy among primary health care physicians in Al-Hasa, Saudi Arabia. J Prev Med Hyg. 2020;61(1):85–91.
- 18. Gilbert C, Gordon I, Mukherjee CR. Guidelines for the prevention and management of diabetic retinopathy and diabetic eye disease in India: A synopsis. Indian J Ophthalmol. 2020;68:S63–66.
- 19. Gale MJ, Scruggs BA, Flaxel CJ. Diabetic eye disease: A review of screening and management recommendations. Clin Experiment Ophthalmol. 2021;49(2):128–145.
- 20. Song P, Yu J, Chan KY. Prevalence, risk factors and burden of diabetic retinopathy in China: A systematic review and meta-analysis. J Glob Health. 2018;8(1).
- 21. Al Alawi A, Al Hassan A, Chauhan D, et al. Knowledge, attitude, and perception of barriers for eye care among diabetic persons registered at Employee Health Department of a Tertiary Eye Hospital of Central Saudi Arabia. Middle East Afr J Ophthalmol. 2016;23(1):71–74.
- 22. Mohammed IM Ahmed, Mawahib AE Abu Elgasim, Mehad AT Mohamed, et al. “Knowledge and Awareness of Diabetic Retinopathy among Diabetic Sudanese Patients, Khartoum State, Sudan, 2018,” Sudan Journal of Medical Sciences. 2021;16(4):476–488.
- 23. Al-Asbali T, Aldawari SA, Alzahim IA, et al. Knowledge, attitude and practice regarding diabetic retinopathy screening and its management among diabetic patients at a private hospital of Riyadh, Saudi Arabia. Saudi J Ophthalmol. 2020;34(2):85–93.
- 24. Qi JY, Zhai G, Wang Y, et al. Assessment of Knowledge, Attitude, and Practice Regarding Diabetic Retinopathy in an Urban Population in Northeast China. Front Public Health. 2022;10:808988.
- 25. Achigbu E, Oputa R, Achigbu K. Knowledge, Attitude and Practice of Patients with Diabetes Regarding Eye Care: A Cross Sectional Study. Open Journal of Ophthalmology.2016;6:94–102.
- 26. Najmi H, Otaif W, Najmi M, et al. Knowledge, Attitude, and Practice around Diabetic Eye Disease among Diabetic Patients in Jazan Region, Saudi Arabia. Middle East Afr J Ophthalmol. 2021;28(2):123–128.
- 27. Venugopal D, Lal B, Fernandes S. Awareness and knowledge of diabetic retinopathy and associated factors in Goa: A hospital-based cross-sectional study. Indian J Ophthalmol. 2020;68:383–390.
- 28. Ahmed MIM, Elgasim MAEA, Mohamed MAT, et al. Knowledge and Awareness of Diabetic Retinopathy among Diabetic Sudanese Patients, Khartoum State, Sudan. Sudan Journal of Medical Sciences. 2018;16(4):476–488.
- 29. Hirakawa TH. Conhecimento dos pacientes diabéticos usuários do Sistema Único de Saúde acerca da retinopatia diabética. Revista Brasileira de Oftalmologia. 2019;78(2):107–111.
- 30. Mwangi MW, Githinji GG, Githinji FW. Knowledge and Awareness of Diabetic Retinopathy amongst Diabetic Patients in Kenyatta National Hospital, Kenya. International Journal of Humanities and Social Science. 2011;1(21):140–146.
- 31. Khandekar R, Harby SA, Harthy HA. Knowledge, attitude and practice regarding eye complications and care among Omani persons with diabetes - A cross sectional study. Oman J Ophthalmol. 2010;3(2):60–65.
- 32. Srinivasan NK, John D, Rebekah G, et al. Diabetes and Diabetic Retinopathy: Knowledge, Attitude, Practice (KAP) among Diabetic Patients in A Tertiary Eye Care Centre. J ClinDiagn Res. 2017;11(7):NC01-NC07.
- 33. Hussain R, Rajesh B, Giridhar A, et al. Knowledge and awareness about diabetes mellitus and diabetic retinopathy in suburban population of a South Indian state and its practice among the patients with diabetes mellitus: A population-based study. Indian J Ophthalmol. 2016;64(4):272–276.
- 34. Khanna RC, Marmamula S, Rao GN. International Vision Care: Issues and Approaches. Annu Rev Vis Sci. 2017;3:53–68.
- 35. Ahmed KR, Jebunessa F, Hossain S, et al. Ocular knowledge and practice among type 2 diabetic patients in a tertiary care hospital in Bangladesh. BMC Ophthalmol. 2017;17:171.
- 36. Al Zarea BK. Knowledge, Attitude and Practice of Diabetic Retinopathy amongst the Diabetic Patients of AlJouf and Hail Province of Saudi Arabia. J Clin Diagn Res. 2016;10(5):NC05–NC8.

