Purpose of Study: To evaluate tear film instability after cataract surgery by measuring tear break up time.
Place of Study: This study was carried out in Teaching Hospital, University of Lahore, Lahore, Pakistan.
Materials and Methods: A descriptive cross- sectional study was conducted in Teaching Hospital, UOL. Tear break up time was measured on patients post-operatively who under -went cataract surgery. A total of 60 patients were included in study after non –probability convenient sampling technique. Both male and female patients were included in study age 45-65 years. Data was collected through self-designed questionnaire based proforma. Further results were analyzed using SPSS version 20.
Results: Tear break up time was found statistically reduced at 1 week, 2 week and after one month postoperatively (P =.0002, P<.0001). However, the tear film stability had reverted to approximately the preoperative measurement 1 month after surgery. The mean values of postoperative results were altered from preoperative measurement values. BUT outcomes had reduced considerably at 1 week postoperatively (P=.0001) but had resumed to very nearly the preoperative value 1 month after of cataract surgery. While goblet cell density (GCD) had reduced considerably at 1 week, 2 week and 1 month postoperatively (P<.0001).
Conclusion: This study concludes that tear breakup time is significantly reduced after cataract surgery due to destruction of goblet cells as shown in above tables. But tear break up time is significantly improved after one week, two weeks and one month of follow ups respectively.
Keywords: Tear film, Cataract surgery, Instability, Phacoemulsification
Modern cataract surgery is one of the most popular and successful surgical procedure carried out today. Despite the satisfactory visual outcomes postoperatively obtained for many patients, some are distracted and dissatisfied due to tear film dysfunction, poor vision, or diminished sensitivity to dissimilarity. Tear film dysfunction because of the use of topical medications, reduced membrane sensitivity, and mucous membrane epithelial cell loss are most generally investigated. Despite ordinary tear production and a usual membrane surface, some patients complain of ocular discomfort.1 Dry eye syndrome is characterized by membrane and mucous membrane xerosis caused by tear deficiency and over evaporation.2 This disease is associated with several ocular symptoms, such as red or watery eyes, sensation of the outside body, and fatigue. It will cause the membrane's organic process, decreased visual sense, and even vision defect. Many ocular procedures are anorectic in the dry eye. In up to 70-80 percent of contact wearers, ocular xerosis have been found. The most common complication of laser-assisted surgery in place of keratomileusis (LASIK) is dryness of eyes postoperatively. During Cataract surgery use of topical drops and ocular surface damage in the eye can also lead to dry eyes.3,4 Dry eye symptoms often arise after triple-crown cataract surgery and persist before successful treatment is adopted in some patients. As a consequence of many variables, once cataract surgery, there may be an impact on the ocular surface atmosphere.
We prefer to test mucous membrane cells by microscopic anatomy (IC) impression, membrane sensitivity and stability of the tear film before and after cataract surgery.5 The goal of the study was to identify possible unhealthy factors that are critical to the occurrence of dry eye after cataract surgery. The tear film consists of three layers: the outermost layer of the super molecule, the intermediate layer of the liquid and the innermost layer of glycol proteins. This classic tear film model originated in the 1950s, and recent studies have modified the model to include proteins that boost stability inside the super-molecular layer. While the role of the tear film layer in dry eye syndrome (DES) is well accepted, due to its advanced structure and mechanisms of action, the tear film remains poorly understood.6 The outer super molecule layer may be a two-layer structure, with an associated inner polar super molecule layer that makes an external nonionic super molecule layer associated with the liquid layer interface that comes into contact with air. Meibomian glands secrete secretion to build the layer of supermolecules and the most lipid supply in the tear film.7 Deterioration of the super molecule layer may result in instability of the tear film, dry disease phase shift, along with an irregular ocular surface, all of which exacerbate DES symptoms. Therefore, in addition to alternative criteria, the state of the super molecule layer of the tear film should be considered during DESS diagnosis and management.8 Schirmer takes a look at the dry eye, tear breakup time (BUT), measurement of tear glycoprotein, epithelial cell count, tear osmolarity, tear enzyme and tonometry, membrane curvature, membrane topography, thickness of central membrane, fundoscopy, and manifest and cycloplegic refractions. Schirmir test was used to measure values. The strip was positioned over one third of the lower palpebra margin over the temporal and medial junction. During the procedure, the patient looked upward to see if possible and typical blinking was allowed throughout the procedure. The strips were detached from the eyes after five minutes and measured the metric linear unit scale imprinted on the sterile strips by calculating the length of the moistened. In order to promote an excellent delivery of dyes, the patient was trained to blink several times.7 The patient was then put for slit-lamp testing and asked to look straight ahead while not blinking.
Below the cobalt-blue-filtered light-weight, the tear film was identified. The interval between the last blink and also the beginning of haphazardly scattered dry spots was accustomed to a timer. However, at each visit, a couple of times was calculated and a mean score was obtained. The most common reason for phase shift dry disease, 20'21 characterized by stagnation of sebaceous gland lipids with or without qualitative/quantitative changes in meibomian gland is preventive sebaceous gland disfunction (MGD). Lipid hypo secretion can result in instability of the tear film, ocular irritation, and ultimately ocular surface disease.8 Multiple ocular and general factors such as contact wear, 23'25 giant inflammation of the process, 26'27 immediate allergy, 28 menopauses, 29'30 and psoriasis 31 are rumored to induce MGD; however, there was no investigation of the impact of cataract surgery on sebaceous gland activity. Inflammation until ocular surgery is involved, one report was printed out. The researchers reported that WHO patients with ocular symptoms had dry eye or inflammation over half an hour of post-laser in position keratomileusis (LASIK) 32. However, they did not identify the inflammation as anterior or posterior (MGD) inflammation, and changes in ocular parameters associated with inflammation were not listed. The aim of this study was to assess whether or not cataract surgery affects the operation of the sebaceous gland and to investigate possible associated changes in the parameters of the ocular surface. Ocular symptoms as well as fatigue of the eyes, discharge, sensation of foreign body, dryness, unpleasant sensation, sticky sensation, pain, epiphora, itching, redness, severe sensation, glare, excessive blinking.9
The main mechanisms of dry eye syndrome are collectively called Tear film instability (DES). The layer of the macromolecule stabilizes the tear film and prevents tear evaporation from the layer of the binary compound tear film. These characteristics of the layer of the macromolecule are also measured based on its thickness, structure and composition. MGD was defined as a persistent, diffuse abnormality of the meibomian glands by the International Workshop on Sebaceous Gland Dysfunction (MGD), unremarkably characterized by terminal duct obstruction and/or qualitative/quantitative changes within the secretion of the organ Macromolecule layer thickness (LLT) may therefore also be a marker of changes in meibum secretion, and measurement of LLT is expected to be helpful for the evaluation and classification of MGDD (obstructive or hypersecretory MGD).10 Dry disease (DED) may be a condition associated with ocular surface changes that causes chronic unpleasant symptoms as well as fatigue, pain, and indistinct vision. Dry eye patients typically have damage to the ocular surface of instinctive tissue and remittent tear secretion, with signs of persistent eye irritation.11 Manual small incision cataract surgery remains the most economical and economical measure of the treatment of cataract patients in developing countries. Even the bottom camp surgeries carried out under the National Vision Deficiency Square Management Program assess mainly manual small incision cataract surgeries. Sight enhancement until cataract surgery is in the midst of appreciable improvements in real-world operations. However, they may have a complication of altered tears that could have a serious effect on the quality of vision and life. This impairs patients' flexibility to perform everyday tasks and may have an effect on job efficiency.12 Dry disease is AN ocular surface condition that causes discomfort due to tear film instability and decreased vision. Within the North American nation, the incidence of dry eye has been reported. The incidence of dry eye among patients attending the patient department in Asian countries was estimated to be about zero.46 percent with a male: feminine magnitude relationship. Cataract is the primary cause of visual impairment worldwide. The most eminent and respected surgery in the field of medicine is cataract surgery at constant times. However, some patients complain of foreign body sensation, pain, redness and blurring of vision when cataract surgery is done, which is perceived to be unintended consequences of the surgery. Some studies have supposed aggravation of dry eye symptoms and signs during cataract surgery (Ram, et al.). Therefore, despite an ideal cataract surgery and a visual acuity, the patients may remain dissatisfied.13
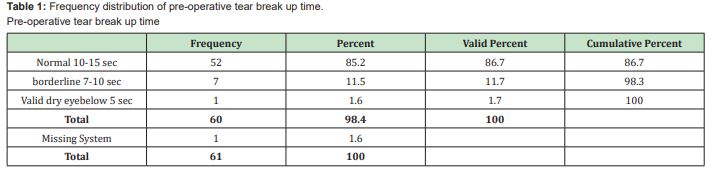
A total of 60 patients were included in study after non –probability convenient sampling technique. Both male and female patients were included in study age 45-65 years. This study was descriptive cross- sectional study in which data was collected from patients who underwent cataract surgery. Pre –operative tear break- up time was measured on patients before cataract surgery by measuring tear break up time of all patients with the help of fluorescein dye strips and slit lamp. Tear breakup time (TBUT) was determined by measuring the interval between instillation of topical fluorescein 0.5% and appearance of the first dry spots on the cornea. Prior to procedure instillation of anesthetic eye drops was done. A fluorescein strip is moistened with saline and applied to the inferior cul-de-sac. Using this procedure tear break up time was measured after one week, two weeks and one month respectively to evaluate the changes in tear film instability. Data was collected through self-designed questionnaire based proforma. Further results were analyzed using SPSS version 20 Further, results were analyzed by using spss version 20. Data was analyzed by applying paired sample t-test.
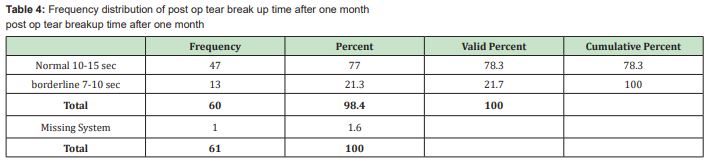
Tear break up time was found statistically reduced at 1 week, 2 week and after one month postoperatively (P=.0002, P<.0001). However, the tear film stability had reverted to approximately the preoperative measurement 1 month after surgery. The mean values of postoperative results were altered from preoperative measurement values. BUT outcomes had reduced considerably at 1 week postoperatively (P=.0001) but had resumed to very nearly the preoperative value 1 month after of cataract surgery. While goblet cell density (GCD) had reduced considerably at 1 week, 2 weeks, and 1 month postoperatively (P<.0001). However, reduction in TUB were significantly correlated with damage of ocular surface during cataract surgery due to use of drugs and incision sites. The findings of this study suggested that goblet cell loss and squamous metaplasia modification of the conjunctival epithelium were higher in patients at 1 week after surgery than at 2 weeks and 1 month after surgery. This confirmed a decrease in the number of goblet cells with increased squamous metaplasia at 1 month after eye surgery, and suggested that one of the main pathogenic factors causing dry eye symptoms following cataract surgery was misuse of eye drops. A reduction in the number of goblet cells was also identified postoperatively, but the significant reduction was greater at 1 week postoperatively than at 2 weeks and 1 month postoperatively Table 1- Table 4 and Figure 1.
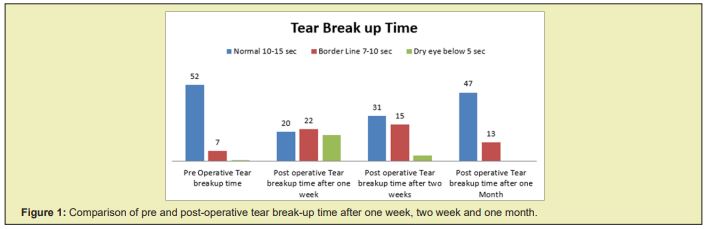
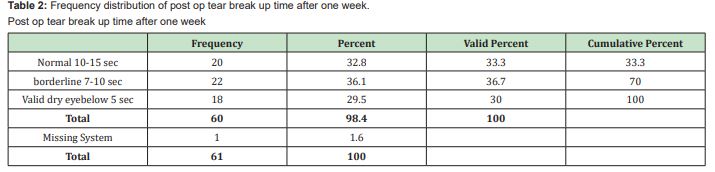
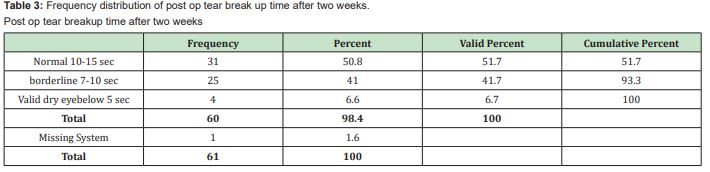
This study shows the symptoms and consequences of dry eye, and damage to the surface of the eye after cataract surgery. Many studies revealed that the dry eye pathogenesis is associated with cataract surgery.14 Li et al. stated that the dry eye syndrome after cataract surgery occurred by the miss use of eye drops. Kohlhaas et al. and Khanal etc. showed that after cataract surgery there was a significant reduction in central corneal sensitivity and this leads to a decrease in tear production. In addition, Ran et al. demonstrated that a small incision made a clear corneal cataract caused a slight decrease in the score and tears. BUT In my study, Partial substantial changes were observed in the corneal tear film permanently after phacoemulsification. After 1 week, 2 weeks and 1 month respectively, corneal tear film stabilization did not return to a steady state, but a trend towards full recovery was seen. It is suspected that decrease in tear breakup time after ocular eye surgery rely on the length of the corneal incision. It would be expected that micro incisional techniques such as cataract surgery would cause less TUB variation than refractive surgery and extra capsular cataract extraction would. Due to limited corneal involvement, postoperative TUB decreases occurred after 1 week, 2 weeks and 1 month in our sample, but restored to near normal levels between 1 and 3 months of surgery. This finding varies from that of an earlier study in which, until 3 months after cataract surgery, TUB did not come back to preoperative levels. The size of the corneal incision made throughout cataract surgery is likely to be linked to this discrepancy. A 2.8mm temporal corneal incision was made in study, while the length of the corneal incision was 4.2mm in the past analysis.15 This would also conclude that the higher the incision duration, the slower the durability of the tear film recovery. In comparison with the pre - operative status, BUT was markedly reduced at 1 week after cataract surgery16 in addition, BUT was enhanced at 2 weeks and 1 month, although still lower than baseline, although. The durability of the tears can be impaired by diffuse corneal sensory nerve damage from surgery such as LASIK, resulting in decreased tear secretion and less blinking.17 For this reason, we may conclude that the misuse of various treatments was not the reason of the reduction of postoperative goblet cells in this sample. In other words, besides the use of eye drops, we can postulate that several causes play a significant role. We found that dry eye indications and conjunctival squamous metaplasia were much more severe for patients with longer operating times. We examined the relationships between operating time and reduction in the number of goblet cells after such studies, and it seemed that the higher the operating time, the more GCD is lowered. It is generally believed that surgical injury, such as cataract surgery, can cause an inflammatory reaction to the ocular surface, including the formation of chemical immune cells such as oxygen-free radicals, proteolytic enzymes and cyclooxygenase. Cho and Kim18 indicated that dry eye signs and symptoms after cataract surgery are exacerbated by microscope light exposure. The longer the operating time, the higher the inflammatory response, which can destroy the ocular surface cells and decrease GCDD. In conclusion, the results of our study show that the symptom score, the durability of the tear film and the actual density of goblet cells were most lessened and slightly improved at 1 week postoperatively, still BUT did not return to the preoperative stage and the indications of the dry eye and the average density of goblet cells return after 1 month postoperatively. Dry eye symptoms are also associated with decreased BUT and goblet cells. Therefore, shortening operating time and reducing other stimuli, such as microscope light exposure, are essential. For cataract patients, prompt and appropriate treatment for dry eye indications, such as artificial tears, autologous serum, and topical cyclosporine A with artificial tears, is important.
This study concludes that tear breakup time is significantly reduced after cataract surgery due to destruction of goblet cells as shown in above tables. But tear break up time is significantly improved after one week, two weeks and one month of follow ups respectively as shown Table 3. Thus, results reveal instability of tear films occurs after cataract surgery. The reduction in GCD, which was associated with surgical time, which almost recover after one month of cataract surgery. Therefore, one of the pathogenic factors causing ocular pain and dry eye disorder after cataract surgery tends to be microscopic ocular surface damage throughout cataract surgery.
None.
None.
The authors declare no conflict of interest during the writing of this article.
- 1. Han KE, Yoon SC, Ahn JM, et al. Evaluation of dry eye and meibomian gland dysfunction after cataract surgery. American journal of ophthalmology. 2014;157(6):1144-1150.
- 2. Apostol S, Filip M, Dragne C, et al. Dry eye syndrome: etiological and therapeutic aspects. Oftalmologia. 2003;59:28–31.
- 3. Sheppard JD. Guidelines for the treatment of chronic dry eye disease. Manag Care. 2003;12:20–25.
- 4. Li XM, Hu L, Hu J, et al. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26:16–20.
- 5. Begley CG, Caffery B, Nichols K, et al. Results of a dry eye questionnaire from optometric practices in North America. Adv Exp Med Biol. 2002;506:1009–1016.
- 6. Oh T, Jung Y, Chang D, et al. Changes in the tear film and ocular surface after cataract surgery. Japanese journal of ophthalmology. 2012;56(2):113-118.
- 7. Green Church KB, Butovich I, Willcox M, et al. The international workshop on meibomian gland dysfunction: Report of the subcommittee on tear film lipids and lipidprotein interactions in health and disease. Invest Ophthalmol Vis Sci. 2011;52(4):1979–1993.
- 8. Shine WE, McCulley JP. Polar lipids in human meibomian gland secretions. Curr Eye Res. 2003;26(2):89–94.
- 9. Knop E, Knop N, Millar T, et al. The international workshop on meibomian gland dysfunction: Report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci.2011;52(4):1938-1978.
- 10. Hardten DR. Dry eye disease in patients after cataract surgery. Cornea. 2008;27(7):855.
- 11. Li XM, Hu L, Hu J, et al. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26(9 Suppl 1):S16-S20.
- 12. Ram J, Gupta A, Brar G, et al. Outcomes of phacoemulsification in patients with dry eye. J Cataract Refract Surg. 2002;28(8):1386-1389.
- 13. Ram J, Sharma A, Pandav SS, et al. Cataract surgery in patients with dry eyes. J Cataract Refract Surg. 1998;24(8):1119-1124.
- 14. Pager CK. Expectations and outcomes in cataract surgery: a prospective test of 2 models of satisfaction. Arch Ophthalmol .2004;122(12):1788-1792.
- 15. Trueb PR, Albach C, Montes Mico R, et al. Visual acuity and contrast sensitivity in eyes implanted with aspheric and spherical intraocular lenses. Ophthalmology. 2009;116(5):890-895.
- 16. Kim J, Chung J, Kang S, et al. Change in Corneal Sensitivity and Corneal Nerve after Cataract Surgery. Cornea. 2009;28(Suppl. 1):S20ėS5.
- 17. Oh T, Jung Y, Chang D, et al. Changes in the tear film and ocular surface after cataract surgery. Jpn J Ophthalmol. 2012;56(2):113-118.
- 18. Sanchez MA, Arriola Villalobos P, Torralbo Jimenez P, et al. The effect of preservative-free HP-Guar on dry eye after phacoemulsification: a flow cytometric study. Eye (Lond). 2010;24(8):1331-1337.

