Background: Obesity is currently considered a public health problem. Bariatric procedures have become an important part of obesity management and, consequently, the number of male patients seeking post-bariatric reconstructive procedures have increased. Therefore, the clinical approach and understanding of the body contour of this population have become more relevant. The goal of post-bariatric reconstruction is to enhance the male silhouette through removal of skin and adipose tissue excess, and abdominal rectus diastasis repair.
Material and methods: We conducted a retrospective study at the Plastic and Reconstructive Surgery Department of the National Medical Center “20 de Noviembre”. All male patients referred to our department to start a post-bariatric reconstruction protocol from January 2018 to December 2022 were included in this study.
Results: In total, 15 patients who underwent corporal contouring procedures were included; median age was 49.2 years with minimum of 33 years, and a maximum of 57 years. Median Body mass index was 28.4 kg/m2 with minimum of 22 kg/m2 and maximum of 38 kg/m2. All patients were treated 18 months after their bariatric surgery. All patients underwent an abdominoplasty as a body contouring procedure. 4 (26.7%) patients presented complications related to the surgery.
Conclusion: We propose a comprehensive and systematic approach to massive weight loss for male patients, suggesting an abdominal marking based on the patient's clinical features and the expected results avoiding feminization of the abdominal body contour.
Keywords: Massive weight loss, Post bariatric, Male, Abdominoplasty, Contouring
According to the American Society of Plastic Surgeons 2,314,720 aesthetic procedures were performed during 2020 with body contouring procedures comprising a significant percentage of them.1 Although male patients represent a minor portion of the overall aesthetic procedures there is an increasing tendency for these patients to seek care from a plastic surgeon (1). Consequently, the approach and understanding of post-bariatric male body contouring is becoming more relevant. Body aesthetic differences, as well as technical-surgical differences, must be recognized to achieve the desired results for the male population. The goals of post-bariatric reconstruction surgery include removal of excess skin and subcutaneous adipose tissue, and abdominal rectus diastasis repair.2
This is a descriptive, observational, retrospective, and cross-sectional study derived from information collected through SPSS version 29 (SPSS Inc, Chicago, IL) with information collected from the electronic medical record of the National Medical Center “20 de Noviembre”. All the male patients referred to our service for the post-bariatric reconstruction protocol from January 2018 to December 2022 were included in this study. The exclusion criteria were patients with incomplete records, weight fluctuations in the last 3 months, a postoperative period less than 18 months since the bariatric procedure, and patients lost to follow-up.
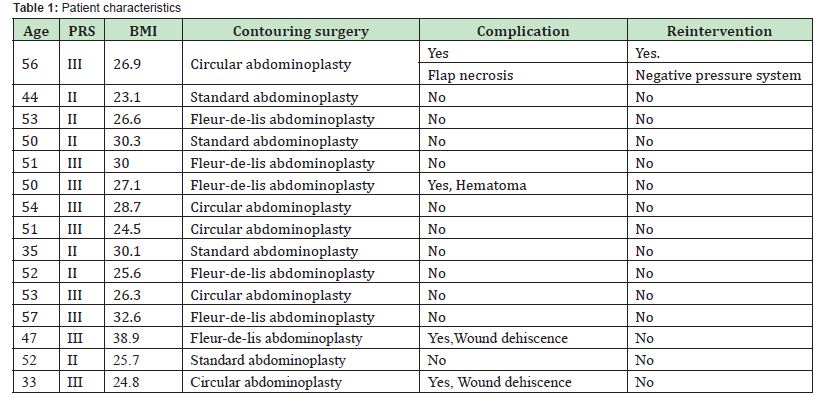
A total of 15 Male patients who underwent a body contouring procedure were included (Table 1). All patients were previously evaluated by the endocrinology service, psychiatry, nutrition, bariatric surgery and later by our service. The minimum age was 33 years and maximum 57 years with a mean of 49 years. 10 patients reported active smoking at the time of the first consultation, however, all 10 patients stopped smoking for at least 4 weeks, 1 patient presented a history of cocaine consumption.
Regarding the technique for the bariatric surgery the most common procedure was gastric bypass practiced on 11 patients, followed by the gastric sleeve practiced on 4 patients.
All patients were approached 18 months after their bariatric procedure and presented a stable weight for at least 6 months prior to their procedure.
All patients underwent abdominoplasty as a body contouring procedure, in 1 case a secondary procedure (torsoplasty) was performed.
Regarding body mass index (BMI) 2 had a normal index, 8 were overweight, 4 had grade I obesity, and 1 patient had grade II obesity. The Pittsburgh Rating Score (PRS) was used to classify abdominal deformity with 6 corresponding to a Pittsburgh II scale, and 9 to a Pittsburgh III scale.
The most performed procedure was the fleur de Lis abdominoplasty in 6, followed by circular abdominoplasty in 5, and the least performed was the standard abdominoplasty in 4 patients.
A closed drain system was used in all the patients, with an output of ≤ 30ml/day as criteria for drain removal, the abdominal wall was closed by layers using absorbable suture material in the subcutaneous layers and monofilament material for skin closure.
4 patients presented a complication related to the surgical procedure, 2 presented dehiscence of the surgical wound, 1 presented hematoma, and 1 presented skin flap necrosis. Only 1 patient required a surgical reintervention due to complications; being required to place a negative pressure system with a subsequent wound closure. The minimum in-hospital stay was 2 days, with a maximum of 8 days, and a mean of 4.2 days. Any death or systemic complication was presented derived from the surgical procedure or during the hospital stay.
Worldwide obesity tripled between 1975 and 2016, according to the World Health Organization in 2016 1.9 billion adults are overweight and more than 650 million were obese.3 It´s estimated that 36.1% of the population over 20 years of age in Mexico is obese.4 Similarly, bariatric procedures have shown a high prevalence, with 198,651 bariatric procedures reported to be performed in the United States of America in the year 2020.5
Due to the increasing prevalence of obesity in recent years, bariatric procedures have become more common and post-bariatric patients are seeking reconstructive procedures. Body contouring surgery after massive weight loss has a positive impact on the patient life quality, so plastic surgeons must be familiar with perioperative management to achieve safe surgeries with satisfactory results.6 Male population still represent a minority in body contouring surgery, consequently plastic surgeons could tend to apply female aesthetic techniques to male patients.7 Given the unique considerations in this group of patients, and a paucity of literature available to guide plastic surgeons, we decided to share our experience in male contouring surgery.
The approach to the post-bariatric patient required a multidisciplinary team integrated by: Clinical nutrition, psychology, internal medicine, bariatric surgery, anesthesiology and plastic and reconstructive surgery.8 Post-bariatric patients should be referred to the plastic and reconstructive surgery service once they meet the following criteria:8
- BMI between 25 to 31 kg/m2.
- Weight loss of at least 50% of excess weight or a loss greater than 45.5 kg.
- No complications of the bariatric procedure (dehiscent wounds, interruption of the digestive tract, etc.).
- A post-surgical period of at least 18 months since the bariatric surgery.
- A stable weight maintained for at least 6 months.
The objective of abdominal contouring surgery in the male is to correct the alterations in the different planes of the abdominal wall: to eliminate the excess skin, to reduce the volume of subcutaneous adipose tissue and abdominal rectus diastasis repair.
There are anatomical differences between both sexes Figure 1, it is essential to keep these differences in mind for the male patient approach. Men have thick skin while women present thin skin with a tendency to laxity and striation. Men tend to present a diastasis of rectus muscles in the upper region, while women present a diastasis of rectus muscles in the lower region. The adipose tissue distribution in women tends to present an hourglass pattern, while men do not present this typical adipose distribution, however they present an accumulation in the flanks (love handles).2

Another important anatomical difference is the position, diameter, and shape of the umbilicus. The mean height of the umbilicus in women is 2.1 ± 0.5 cm and in men 2.1 ± 0.7 cm. The mean width of the umbilicus in women is 2.4 ± 0.7cm, and in men 2.1 ± 0.6 cm. The mean distance from the lower edge of the umbilicus to the upper edge of the pubis is 14.1 ± 2.1 cm in men and 13.8 ± 1.4 cm in women.9
The aesthetic standards in men differ, a silhouette with broad shoulders and a narrower hip is expected, conditioning an inverted cone silhouette, while in women an hourglass silhouette with a narrow waist, broad shoulders and hips is expected.10
The female body shapes are curvaceous and soft, while the male shape is more angular, in which the upper silhouette of the body predominates (10). The female inframammary fold presents a smooth and circular shape, while ideally in men it should be barely visible due to the poor development of the mammary gland.10
Male patients have been associated with increased risk of psychosocial dysfunction in aesthetic surgery populations, with a tendency toward more unrealistic expectations about surgical outcomes when compared with female patients. Male gender has been associated with increased risk of total complications and major complications following abdominoplasty or panniculectomy.11
Complications are expected in this population, up to 25% of patients who undergo a single procedure present a complication, if procedures are added the risk increases up to 50%. The 2 most common complications are wound dehiscence (10% for single procedures and 30% for multiple procedures) and seroma (4% for single procedures and 19% for multiple procedures).12 Another point to consider is gender, an increase in the formation of seromas and hematomas has been observed in the male patient, so it is advisable to warn this population about this risk.13
Nowadays insurance coverage of post-bariatric abdominal contouring procedures remains inadequate in coverage policy criteria among insurance providers.14 Insurance companies often have opaque policies, which make accessing treatment and gaining reimbursement difficult.15
The marking Figure 2 is performed one day before the surgical procedure in the outpatient consultation with the patient standing. It begins by marking the abdominal midline by drawing a line from the sternal manubrium to the base of the penis, routinely marking the costal margin.
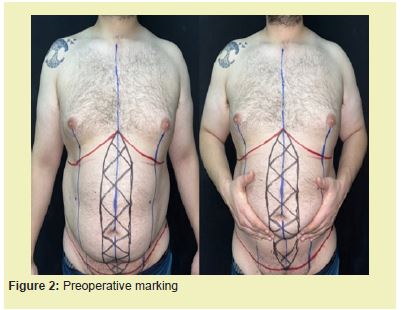
We ask the patient to gently retract the skin flap without excessive traction. We mark 6 centimeters above the base of the penis, then we extend 6 centimeters horizontally bilaterally, and from that point we direct a diagonal line towards the anterior superior iliac spines. For the marking of the plication of the rectus muscle we start from the abdominal midline and extend 4 centimeters horizontally bilaterally, extending superiorly and inferiorly; the plication is conservative to avoid its feminization.
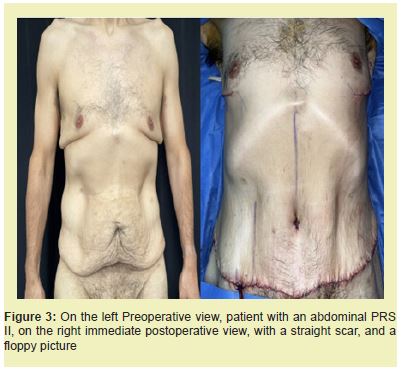
The limits of resection of the excess skin flap are individualized intraoperatively by pulling the flap conservatively caudally, then the excess skin is cut off, avoiding tension and displacement towards the midline to prevent the accentuation of the waistline Figure 3.
Male abdominal body contouring in patients with massive weight loss presents specific challenges for the plastic surgeon, since most of the described techniques have focused on female body contouring. It is essential to individualize each patient, understand the anatomical differences with respect to the female contour, physical characteristics, weight loss, and correct surgical planning to achieve favorable aesthetic results.
All procedures performed in studies involving human participants were in accordance with the ethical standard of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
All patients signed informed consent for surgery, use of photographs and data for publication.
None.
This Research Article received no external funding.
Regarding the publication of this article, the authors declare that they have no conflict of interest.
- 1. The American Society of Plastic Surgeons. Plastic surgery Statitics Report. ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. USA. 2020.
- 2. Matarasso A. The male abdominoplasty. Clin Plast Surg. 2004;31(4):555-569.
- 3. Obesity and overweight. Who.int.
- 4. Instituto Nacional de Salud Pública (MX). Encuesta Nacional de Salud y Nutrición [National Health and Nutrition Survey 2018]. Cuernavaca, México. 2018.
- 5. ASMBS. Estimate of Bariatric Surgery Numbers [Internet]. American Society for Metabolic and Bariatric Surgery. 2023.
- 6. Telich Vidal J, Ramírez Sosa LE, Ángeles Gaspar D, et al. Cirugía postbariátrica: el último eslabón en el protocolo de cirugía metabólica. Cirugía Plástica. 2020;30(3):172-179.
- 7. Hurwitz D. Enhancing Masculine Features After Massive Weight Loss. Aesthetic Plast Surg. 2016;44(4):245-255.
- 8. Portes Castro A, Morales Olivera JM, Corona García R, et al. Clinical guidelines for the interdisciplinary management of patients with sequelae of massive weight loss during reconstructive plastic surgery. Cir Plast Iberolatinoam. 2016;42(1):77-91.
- 9. Yu D, Novicoff WM, Gampper TJ. The Average Size and Position of the Umbilicus in Young Men and Women. Ann Plast Surg. 2016;76(3):346-348.
- 10. Zarins U, Sandis K. Anatomy for sculptors: understanding the human figure”. Anatomy Next, Incorporated. 2015.
- 11. Donato DP, Simpson AM, Garlick JW, et al. Abdominal Contouring and Male Gender: Analysis of Complications Using the National Quality Improvement Program Database. Ann Plast Surg. 2019;83(4):481-487.
- 12. Gusenoff, Jeffrey A. Managing Body Contouring Challenges and Complications. Springer. 2019.
- 13. Chong T, Coon D, Toy J, et al. Body Contouring in the Male Weight Loss Population. Plast Reconstr Surg. 2012;130(2):325e-330e
- 14. Ngaage LM, Elegbede A, Pace L, et al. Review of Insurance Coverage for Abdominal Contouring Procedures in the Postbariatric Population. Plast Reconstr Surg. 2020;145(2):545-554.
- 15. Ngaage LM, Wasicek PJ, Puthumana J, et al. A Cross-sectional Analysis of Insurance Coverage of Extremity Contouring After Massive Weight Loss. Ann Plast Surg. 2020;84(3):253-256.

