Introduction: Maxillo-Orbito-facial tissue loss represents a multifaceted category of lesions encompassing skin, muscle, mucosa, and bone. Diverse reconstruction techniques are employed to address this challenge. This study aims to comprehensively explore the epidemiological, diagnostic, and therapeutic facets of maxillo-Orbito-facial substance loss.
Materials and Methods: This retrospective, cross-sectional, observational, descriptive, and analytical study was conducted at a single-center, the Department of Stomatology and Maxillofacial Surgery, from March 2016 to March 2022. The study included patients who underwent maxillofacial reconstruction due to substance loss, with the exclusion of cases lacking complete medical records. We examined the following parameters: frequency, age, gender, occupation, socioeconomic status, time of consultation, etiological factors, radiological assessments, treatment modalities, surgical techniques, complications, and long-term consequences.
Results: 74 patients were included. The mean age was 31.9 years with a sex ratio of 1.96. Active patients accounted for 44.6% of cases. 74.4% of patients lived in urban areas. Traumatic substance loss accounted for 66.2% of cases. Autologous reconstruction was performed in 59.5% of cases. Consequences were found in 6.8% of cases.
Conclusion: Losses of maxillo-Orbito facial tissue are the prerogative of young men. They are mainly of traumatic origin. Autologous reconstruction is the most commonly used technique.
Keywords: Substance loss, Maxillo-orbito-facial, Epidemiology, Therapeutics, Gabon
Maxillofacial tissue loss encompasses a wide spectrum of multi-tissue lesions affecting the skin, muscle, mucosa, and bone. Such tissue loss often arises as a consequence of tumor removal, trauma, infection, or radionecrosis. Maxillo-orbito-facial tissue loss is a prevalent condition, particularly among young individuals, and can significantly impact vital functions, such as mastication, speech, respiration, and vision.1 Reconstructing these tissues presents a formidable challenge in the field of maxillofacial surgery, owing to the intricate osteo-architecture and the presence of vital organs in this anatomical region. Multiple reconstruction techniques are employed, including local flaps, implants, avascular and vascularized bone grafts, and micro-anastomosed flaps.2
The primary objective of our study is to provide a comprehensive review of the epidemiological, diagnostic, and, most importantly, therapeutic aspects associated with maxillo-orbito-facial tissue loss.
This study is a single-center retrospective, cross-sectional, observational, descriptive, and analytical investigation conducted from March 2016 to March 2022 at the Department of Stomatology and Maxillofacial Surgery. It enrolled patients who underwent maxillofacial reconstruction due to substance loss while excluding cases of congenital substance loss, substance loss without reconstruction, and those with incomplete medical records. The study comprehensively analyzed several key parameters, including the frequency of cases, patients' gender, age, occupation, social status, time of consultation, etiological factors, treatment modalities, surgical techniques, complications, and sequelae. To process the collected data, Microsoft Excel and XLSTAT 2022 software were employed.
Epidemiological findings
Frequency
Among the 1,075 patients admitted to the department during the study period, 74 cases were identified, representing a hospital frequency of 6.9%.
Age
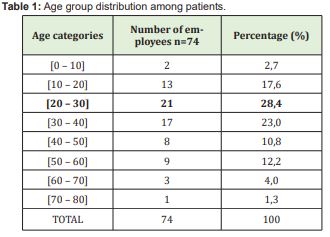
The mean age of the patients was 31.9 years, with a range of 1 to 72 years. The age group of 20-30 years accounted for the highest number of cases at 28.4% Table 1.
Out of the cases, 66.2% were male, and 33.8% were female, resulting in a sex ratio of 1.98.
Occupation
The patients' occupations varied, with 44.6% being workers, 35.1% learners, 12.2% unemployed, and 8.1% pensioners.
Consultation period
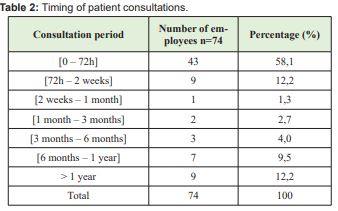
A majority of patients (58.1%) sought medical consultation within 72 hours, while 12.2% consulted within 72 hours to 2 weeks, and an additional 12.2% consulted within one year Table 2.
Etiology
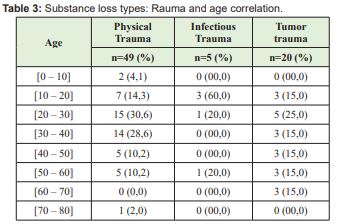
The etiology of substance loss was as follows: Physical trauma was responsible for 66.2% of cases, with 20 cases (27%) originating from tumor excisions and 5 cases (6.8%) stemming from infectious causes. Examining the distribution across age groups, physical trauma constituted 30% of substance loss cases within the 20-30 age group Table 3. When analyzed by gender, male patients accounted for 69.4% of substance loss cases due to physical trauma, 80% of cases were related to infectious trauma, and 55% were attributed to tumor trauma. In contrast, female patients had substance loss due to physical trauma in 30.6% of cases, infectious trauma in 20%, and tumor trauma in 45% of cases.
Seat of substance loss
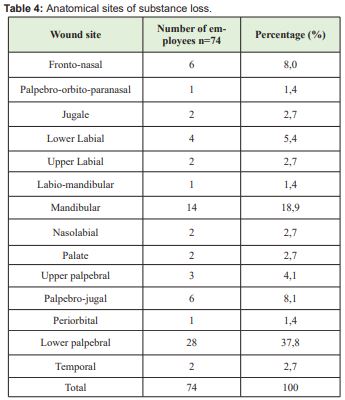
Loss of substance predominantly occurred in the inferior palpebral area (37.8%), with a small percentage affecting the upper palpebral region (4.1%) and the mandibular area (18.9%) Table 4.
Radiological assessment
The diagnostic tools used included CT scans in 51.4% of cases, panoramic dental X-rays in 24.3%, Blondeau X-rays in 12.2%, and 12.1% of cases lacked X-ray assessments.
Therapeutic aspects
Reconstruction methods
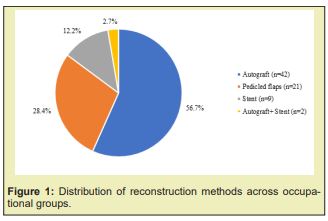
Autologous transplants were utilized in 59.5% of cases, and a combination of autologous transplants and stent grafts in 2 cases Figure 1.
Stent
Stents were used in 14.8% of cases, with the Krenkell splint employed in 36.4% and mesh plates in 63.6% Figure 2.

Autologous Transplant
Bone reconstruction utilized iliac bone in 47.7% of cases, conchal ear cartilage in 38.6%, and rib bone in 13.6% Figure 1.
Flaps
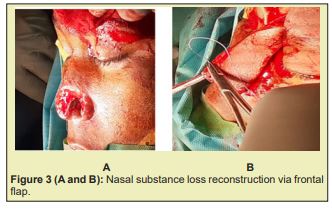
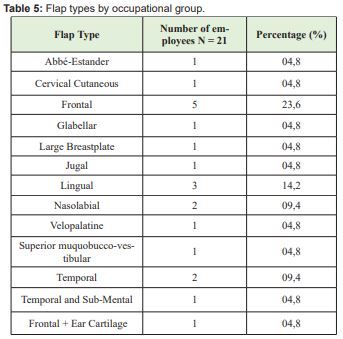
Frontal flaps were performed in 23.6% of cases, lingual flaps in 14.2% Figures 3 (A and B) and temporal flaps in 9.4% Table 5.
Complications
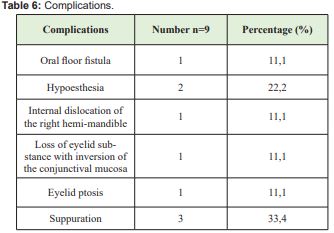
Most cases (87.8%) had an uncomplicated course, while 12.2% experienced complications Table 6.
Aftermath
Sequelae were observed in 6.7% of cases, including swallowing and speech disorders (40%), hypoesthesia of the hemiface (40%), and blurred vision (20%).
Frequency
Over a 6-year period, we identified a total of 74 cases involving acquired loss of maxillo-orbito-facial substances, resulting in an annual frequency of 6.9%. This annual incidence is notably lower than the 12.4% reported by Diallo.1 Notably, the months of October and November stand out as having the highest incidence of substance losses, with rates of 7.6% and 8.8%, respectively. These peaks align with the beginning of the school year, coinciding with increased road traffic and a heightened risk of traumatic substance loss.
Age
The mean age within our study cohort stands at 31.9 years, with the most prominently affected age group being 20 to 30 years, constituting 28.4% of cases. These findings closely align with the research conducted by Diallo,1 who reported an average age of 28 years and identified the 21 to 30-year age goup as the most affected. However, our results deviate significantly from those reported by Beogo in Burkina Faso3 and Donkor in Ghana,4 who identified average ages of 26.6 years and 36 years, respectively, among their study populations.
Sex
Within our series, males predominate, accounting for 66.2% of cases, resulting in a sex ratio of 1.96. This finding closely aligns with the research by Diallo in Guinea Conakry in 2012, where they reported 74.3% of cases being male,1 as well as the work by Mansouri in Morocco in 2012, which identified 72% of cases as male.5 This male predominance can be attributed to the fact that men are often exposed to higher levels of trauma due to their engagement in risky activities and behaviors, such as sports, dangerous driving, contact sports, among others.
Occupation
A significant portion of the patients in our study are actively employed, comprising 44.6% of the cases, followed closely by learners, including pupils and students, at 35.1%. These findings correspond with the observations made by Njimah in Douala.6 Notably, the most frequently encountered socio-professional categories are manual workers, accounting for 19.7% of cases, and motorcycle taxi drivers, representing 17.7% of cases.
Consultation period
A noteworthy 58.1% of patients in our study sought medical consultation within 72 hours of the onset of symptoms, primarily associated with traumatic substance losses. This finding closely mirrors the observations made by Millogo in 2022, who identified a delay of 2 to 4 days in 50% of cases for traumatic substance losses. In some instances, consultation times exceeding 6 months can be attributed to the gradual progression of benign tumors.
Etiology
In our study, trauma emerges as the predominant etiological factor, accounting for 66.2% of cases. This aligns closely with the findings of Millogo,7 who identified trauma as the primary etiology in 80% of cases.
Seat of substance loss
The lower eyelid is the predominant site, accounting for 37.8% of cases, while the mandibular region is involved in 18.9% of cases. This observation is consistent with the findings reported by L Azoulay8 where they also noted a predominance of the lower eyelid as the primary site of substance loss in 85.7% of cases. This area is frequently exposed to trauma during accidents, thus explaining its higher prevalence.
Radiological assessment
The most frequently utilized radiological examination is CT, performed in 51.4% of cases, followed by panoramic dental X-rays at 24.3%. Blondeau X-rays were used in 12.2% of cases. This preeminence of CT aligns with the findings reported by Salimata Camara9 where it was exclusively used in 100% of cases. Additionally, 12.1% of cases lacked X-ray assessments, typically associated with the loss of soft tissue substances without bone substance involvement.
Therapeutics: Reconstruction methods
Substance loss reconstruction in our study employs a variety of techniques, with autografts being the most commonly used method in 56.7% of cases, followed by flaps in 28.4% of cases, stents in 12.2% of cases, and a combination of autografts and stents in 2.7% of cases. The selection of these methods is contingent on several factors, including the location and cause of substance loss, as well as the specific type of loss. Notably, our findings diverge from those of Millogo in 2022, where flaps were the preferred method for substance losses, used in 48% of cases.
When it comes to reconstructing bone substance losses using autografts, the iliac bone is the preferred choice in 47.8% of cases, while the concha of the ear is used in 38.6% of cases, and costal bone in 13.6% of cases. This utilization of the iliac bone aligns with the findings of LB Moura in 2016, where it was employed in 76.1% of cases.10 The iliac bone is particularly indicated for reconstructions involving bone loss of the orbital floor. In cases of mandibular bone reconstruction, rib grafts are typically employed, while free fibula reconstruction using the Lambo technique is utilized in 29% of cases by C. d'Hauthuille11 Additionally, there are instances where custom-made three-dimensional implants, designed using software, are employed for reconstruction.12
In our study, the use of pedunculated flap techniques primarily involves the frontal flap in 23.8% of cases, followed by the lingual flap in 14.2%, and the temporal flap in 9.4% of cases. These results are consistent with the observations of Fazil Apaydin13 who found that the paramedian frontal flap is a dependable choice for reconstructing substantial nose defects. Stents were utilized in 11 out of 74 patients, constituting 14.9% of cases. Among these patients, 63.6% received a mesh plate, while 36.4% were fitted with a Krenkell splint. The use of a mesh plate was predominantly associated with cases involving traumatic loss of bone substance. The Krenkell splint, on the other hand, plays a pivotal role in the reconstruction of the mandible when the loss of bony substances is attributed to tumorous or infectious origins. It serves as the initial step in a two-stage reconstruction process.14
Patient progress
In the majority of cases, the post-operative follow-up shows uncomplicated progress, with 87.8% experiencing straightforward recoveries. Nonetheless, in 12.2% of cases, complications such as suppuration, visual blurring, as well as swallowing and phonation disorders were encountered. Irrespective of the chosen technique, whether grafts, flaps, or stents, the post-operative course generally remains quite satisfactory. This outcome is notably better than the 28% complication and sequelae rate reported by B Devauchelle.15
Our study highlights the impact of maxillo-orbito-facial substance losses, particularly in young males, primarily caused by trauma followed by tumors. The diverse reconstruction techniques, including autografts, flaps, and stents, offer effective solutions. Fortunately, most patients experience positive post-operative outcomes.
None.
None.
The author declares no conflicts of interest regarding the publication of this paper.
- 1. Diallo OR, Camara SAT, Diallo A. et al. Traumatic cervicofacial wounds at the Donka National Hospital of the University Hospital of Conakry. Mali Med. 2012.
- 2. Jalbert, Alpy A, Fenelon M, et al. Simulation of implant reconstruction on fibula flaps: evaluation of the use of surgical guides. 63rd SFCO Congress. 2015.
- 3. Beogo R, Konsem T, Ouedrago WF, et al. Repair of mandible loss of substance interrupting substance by non-vascularized bone graft after ablative surgery of benign lesions at Souro Sanou University Hospital: Preliminary results. Odonto-Stomato Afr Chir Maxillo-fac. 2010.
- 4. Donkor P, Bankas DO, Boakye G, et al. The Use of Free Autogrnous Rib Grafts in MaxilloFacial Reconstruction. Ghana medical journal.2006;40(4):127-131.
- 5. Mansouri HN, Lahmiti S, EI Bouihi M, et al. Facial wounds: an epidemiological review of 850 cases. Journal of Stomatology and Maxillofacial Surgery. 2011;112(3):135-138.
- 6. Njimah AN, Bella F, Vodouhe U, et al. Traumatic ENT and head and neck lesions at Laquintine Hospital in Douala: Epidemiological and clinical aspects on a series of 299 cases. Health sciences and disease. 2019;20(3).
- 7. Millogo M, Sanfo M, Idani M, et al. Loss of maxillofacial substances of traumatic origin at Yalgado Ouedraogo University Hospital. Annals of Aesthetic Plastic Surgery. 2022.
- 8. Azoulay L, Prudhomme A, Gleizal A, et al. Use of the autologous dorsal dermis in posterior palpebral lamellar reconstruction in blepharopoiesis. Annals of Aesthetic Plastic Surgery. 2019;64(1):44‑53.
- 9. Salimata Camara. Reconstruction of losses of ballistic mandibular bony substances. USTTB.2021
- 10. Moura LB, Carvalho PH de A, Xavier CB, et al. Autogenous non-vascularized bone graft in segmental mandibular reconstruction: a systematic review.Int J Oral Maxillofac Surg. 2016;45(11):1388‑1394.
- 11. d'Hauthuille C, Testellin S, Maure C. et al. Mandibular Osteoradionecrosis: Part II: Efficacy of Revascularization Surgery. Rev Stomatology and Maxillofac Surgery. 2008;109(5):296-300.
- 12. Albert S, Cristofari JP, Cox A. et al. Mandibular reconstruction by microanastomosed fibula flap. Preoperative radiological modelling using Osirix software. Annals of Aesthetic Plastic Surgery. 2011;56(6):494-503.
- 13. Apaydin F. Lateral crural turn-in flap in functional rhinoplasty. Archives of facial plastic surgery. 2012;14(2):93-96.
- 14. Aka GK, Kouakou RK, Djemo BR, et al. Facial rehabilitation with maxillofacial prostheses in benign tumors of the mandible. Ivorian Journal of Odonto-Stomatology. 2006;8(2):39-48.
- 15. Devauchelle B, Testellin S, Dakpe S. et al. The Iliac Odyssey “Mandibular reconstruction by autotransplantation”. Annals of Aesthetic Plastic Surgery. 2021;66(3):193-200.

