Workers’ compensation (WC) was introduced as a no-fault system to provide injured workers with timely access to medical treatment and compensation for lost wages. When the treating physicians submit a care request to the third party insurer, these requests are often subjected to a utilization review process. Utilization Review (UR) is the process of comparing an injured worker’s case to evidence-based clinical guidelines that outline national standards for a patient with similar symptoms as the one being reviewed. UR often results in a delay or denial of treatment and access to care. Analyzing these disparities can help improve patients' access to appropriate and necessary medical care. A retrospective case series was utilized to analyze existing treatment plans of multiple patients subjected to the UR process. Consent was obtained from an orthopedic private practice located in the Greater Chicago Area to review a series of anonymous WC patient histories. Between January 1, 2024, to December 1, 2024, a total of 42 WC patients were subjected to the UR process. For each patient, their insurer, type of requested treatment, and dates of each UR denial were tracked. Then, the frequency of the total number of UR repeat submissions, total denials, and total approvals pertaining to each requested treatment type was collected. The analyzed requested treatments included the following: pharmacy, physical therapy, surgical, and durable medical equipment. The results displayed that 93.75% of the 42 patients’ UR submissions were denied with these patients facing a longer wait time of 124 days and more frequent UR resubmissions.
Keywords: UR process, Rehabilitation, Chicago, Medicine, pharmacy, Physical therapy
Workers’ compensation was introduced as a no-fault system to provide injured workers with timely access to medical treatment and compensation for lost wages.1 The first introduction of workers’ compensation (WC) can be traced back to 1838 in Germany, when the Prussian Railway Liability Act held railroads responsible for injuries sustained by passengers or employees. Then, in 1884, Germany enacted a comprehensive WC law that covered employees of certain industries against major injuries and shifted all government-provided work relief onto the employer.2 In the United States, WC laws were first constructed during the early 1900s following the industrial revolution and a remarkable increase in injuries that came along with new industrial jobs. Before the implementation of WC, those who were injured at work often had no means of seeking treatment and compensation for lost work days from their employer or coworkers.3 In current times, a WC claim begins when an employee who has been injured at work files for workers' compensation and visits a physician. The physician then submits a care request that then awaits authorization from the third-party insurance provider.4 Although WC was developed as a no-fault system of care, insurance companies often limit access to appropriate medical care through a system of denial. Such denials are decided upon through preliminary review processes, specifically, utilization review. Utilization Review (UR) is the process of comparing an injured worker’s case to evidence-based clinical guidelines that outline national standards for a patient with similar symptoms as the one being reviewed.5 Such clinical guidelines include the Official Disability Guidelines (ODG), which are the most widely used guidelines in the WC industry.6 Section 8.1a of the Illinois Workers Compensation Act mandates that an insurance company that utilizes UR must use a similarly trained physician and an accepted national treatment guideline to review the recommended treatment. The treating physician may then respond via phone call or in written fashion to provide their clinical reasoning as to why they feel their care is necessary and appropriate. If the insurance company disagrees with the treating physician’s response, they may then invoke a new UR physician using accepted national standards.7 In a 2001 study published in the Journal of Risk and Insurance, researchers found that the rate of workers’ compensation claims decreased as a result of more aggressive denial policies.8 With increasing denials, individuals injured at work through no fault of their own are left without access to the necessary care recommended by their treating physician. Taken together, these factors depict a scenario that is ripe for research to further the idea that change can be facilitated to support the treatment plans of workers’ compensation patients.
Disparities and access to healthcare
The recent increase in denial raises questions about the possible disparities presented in this process. For example, as noted by Tulane Law Professors in their 2022 study, populations of those living in rural areas and persons of color have increased difficulties accessing proper health care. Such issues produce disparities in health care.9 According to a 2024 study published in the Journal of Occupational Rehabilitation, factors influencing access to proper healthcare services can be impacted by characteristics like age and gender, degree of injury, occupation, and insurance provider.10 Concurrently, challenges in obtaining workers’ compensation case authorizations emphasize the difficulty many patients face in accessing appropriate and timely treatment. Moreover, Social Insurance Officers can increase denial rates through restrictions of eligibility requirements. Although these restrictions lower costs of the program through decreasing the amount of money billed out for patient care, increasing denial rates discourage patients from filing a workers’ compensation claim.9 In addition to this idea, David Card, a recipient of the Nobel Prize in Economics, and Brian McCall, a professor of economics at the University of Michigan, write in their ILR Review published article that employers are more likely to deny liability for uninsured workers in comparison to insured workers. This finding displays possible bias towards those without access to healthcare and underscores the need for more research on the workers’ compensation process.11 Advancing upon the idea of these eligibility requirements, utilization review incorporates similar processes.
Decreasing costs of workers’ compensation
Insurance providers deny claims for a multitude of reasons, such as exaggeration of losses or concerns over fraudulent claims, which could raise insurance costs as well as costs reflected on to the consumer. As shown through the aforementioned study conducted by David Card and Brian McCall, fraudulent claims are present within the WC process given their findings revealed that 18% of WC claims are post-dated by the injured worker so that the date of injury lands on a Monday. Although there are scenarios in which fraudulent WC claims appear, WC costs have been trending downward. According to a 2015 ProPublica study on the loss of WC benefits, for every $100 of Illinois workers’ wages, the average WC cost to Illinois employers has decreased from $3.58 in 1988 to $2.35 as of 2014. This information marks a $1.23 decrease in the costs of WC over 26 years.12 Reinforcing this point, the National Council on Compensation Insurance (NCCI) stated that the frequency of WC claims over $1 million has decreased by 3% each year since 2002; therefore, it is suggested that WC costs have been trending downward.13 Since large claims drive a substantial portion of total WC costs, their declining frequency would contribute to an overall decrease in WC expenses. In addition to this data, a Statista graph displays that the value of WC benefits has decreased from $14.41 billion in 2004 to $11.78 billion as of 2020 in the United States.14 The data proposed by ProPublica, NCCI, and Statistica negates the concerns of many insurance companies surrounding runaway insurance costs since WC costs have been decreasing over the past years.
Utilization review
Another factor contributing to the rate of denials for workers’ compensation patients is the Utilization Review process. Utilization review (UR) is the process in which care requests are compared to nationally-based guidelines, or clinical guidelines, for symptoms and care plans of similar injuries. The goal of UR is to decide whether or not the request fits within the criteria set by clinical guidelines. Dr. Lee Glass, an occupational medicine specialist, notes that UR must be used in a “flexible manner with attention to the realities of each specific case.”15 This detail of the ideal utilization review process presents an underlying issue in which nationally set standards are far too general to apply to the individual cases of each WC patient, and such instances may lead to the increasing denial rates. To connect to this observation made by Dr. Glass Lee, a meta-analysis published in the Journal of Occupational Rehabilitation in 2024 provides an overview of the need for lessened policies limiting healthcare access. These limits negatively impact patients’ access to proper care, their frequencies of returning to work, and recoveries. The article also highlights that 13.3% of workers in the United States have faced “some or a lot of difficulty getting medical care” following their injury. In California, 8.5% of workers struggled to access physical therapy, 7.9% encountered difficulty finding specialty care, and 2.5% struggled with receiving prescription medications.10
Location of workers’ compensation claims
Chicago, Illinois, is an ideal location to research due to its concentrated population of workers’ compensation patients. A 2017 annual report of Illinois WC claims displays that of the approximately 45,000 WC claims made in Illinois each year, over 17,000 of them are made in Chicago.16 Chicago's significant number of WC claims not only creates an impact on the state, but also on a national and international level, seeing as Chicago is a hub for trade and commerce. In addition to the location of a medical practice, the specialty of said practice also plays a part in identifying proper data on workers’ compensation claims. For example, orthopedic surgeons, who operate specifically on patients with musculoskeletal injuries or diseases, come into contact with a large number of workers’ compensation cases due to the prominence of musculoskeletal injuries in job-related instances.17 Specifically, as noted by a study that took place from 2007 to 2008 and analyzed the financial information related to WC patient care, WC represents 12% of orthopedic surgeons’ annual revenues.18
A gap within the pre-existing research on workers’ compensation centers around quantitative data on why denials are given to WC patients undergoing orthopedic treatment. The usage of clinical guidelines as a comparative counterpart for the individual care requests of each patient highly generalizes the process of WC case reviews and should be further studied. As stated by a 2020 article from the Journal of Occupational and Environmental Medicine, more research needs to be done on the efficiency of utilization review, as well as patient outcomes and costs.5 For example, the efficiency and accuracy of the nationally set requirements utilized in the utilization review process require further evidence collection. Regarding UR and its effects on WC authorization, there is limited evidence addressing this issue in private surgery centers, and even less data specific to the city of Chicago, Illinois. In addition, more research needs to be done to address increasing WC denial rates in the orthopedic setting.
Research question
Due to the prominence of WC patients in Chicago and the large number of WC patients that visit orthopedic surgeons, the research process has revealed that this location requires more data collection on how utilization review impacts the WC process. Thus, the following question arose: In what ways do insurers’ utilization review processes hinder Chicago-based workers' compensation patients from accessing care? Addressing this question will help to fill a gap in the existing research on utilization review and its impact on denials for workers’ compensation patients.
The most effective method to collect an accurate scope of the data surrounding workers’ compensation denials would be a retrospective case series, which would analyze existing treatment plans of multiple patients. Case series are popular forms of data collection in the healthcare field, as shown by a case series that took place from November to March of 2020 and was published in BMC Infectious Diseases. This article tracked data on demography, clinical presentation, treatments, and outcomes of treatments of children admitted to a tertiary care hospital in Germany.19 Another form of case evaluation research is also seen in Robert Hamm's study, which evaluated the cases of 185 WC patients reviewed in 1998 and 1999. This study tracked whether the case evaluations done by the respective WC case examiners were adequate, superficial, or had no treatment at all. The study revealed that the majority of these cases were deemed to have had superficial case evaluations, meaning case evaluations that were inadequate and solely focused on a patient’s chief complaint and manifest symptoms.20 Despite differing patient demographics, both of the aforementioned studies utilized case series to navigate individual treatment plans in which each patient underwent different treatment plans. Commonly in the medical field, case analyses are utilized to assess patients’ access to care; therefore, a case series following multiple workers’ compensation patients was the best form of data collection.
Locating a practice
A retrospective case analysis focusing on patients whose recommended treatment was subjected to the utilization review process was used to identify the possible pitfalls of the utilization review process. To begin this methodology, the researcher used their personal network and obtained consent from an orthopedic private practice located in the Greater Chicago Area to review a series of anonymous patient histories. These documents pertaining to the UR submission histories of patients included WC patients from January 1, 2024, to December 1, 2024. In order to maintain patient confidentiality, the documentations were removed of any patient identifiers prior to the researcher’s review.
Data collection
Between January and December 1 of 2024, a total of 42 WC patients were subjected to the UR process at the identified practice. For each patient, their insurer, type of requested treatment, and dates of each UR denial were tracked. Then, the frequency of the total number of UR repeat submissions, total denials, and total approvals pertaining to each requested treatment type was collected. The analyzed requested treatments included the following: pharmacy, physical therapy (PT), surgical, and durable medical equipment (DME). Additionally, the average wait time of each denied treatment, dating from the oldest UR submission date to the most current response from the insurance company, was recorded. For any approvals, the dates of approval and whether or not it was paid were also recorded.
The Illinois workers’ compensation act mandates that an insurance company that utilizes UR must use a similarly trained physician and an accepted national treatment guideline to review the recommended treatments. To assess this information, the clinical guideline used by each insurer was tracked.
Data analysis
Once the data was collected, the frequency of denials and approvals were analyzed. The average number of UR resubmissions for each insurance provider was also calculated. Another set of analyzed data points included the total denial and approval rate, as well as the percentage of insurers who utilized the official disability guidelines. Finally, the standard deviation of wait time was recorded.
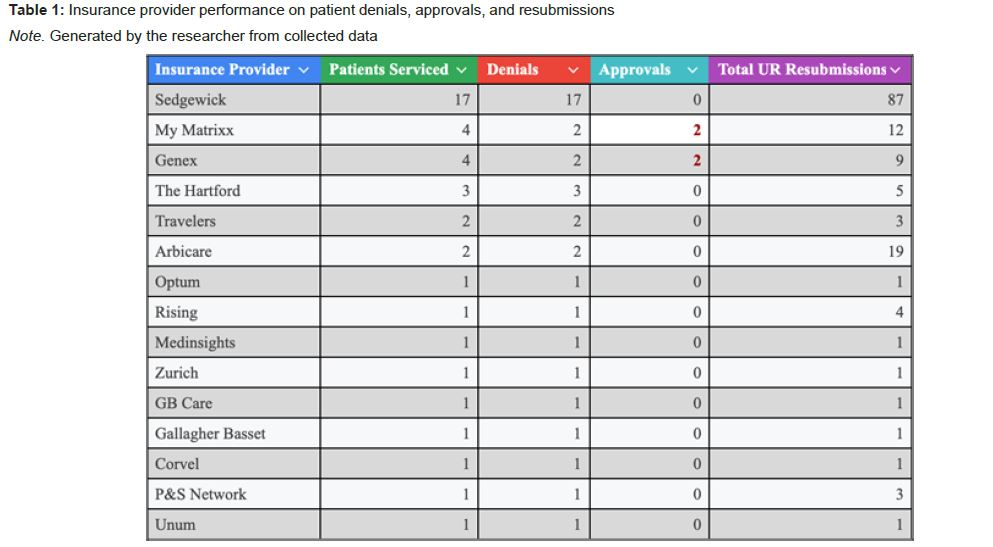
Insurance provider denials
The total number of insurance companies tracked among the 42 patients was fourteen. The insurer with the greatest number of denials was Sedgewick, with seventeen denials. The insurer with the second greatest amount of denials was The Hartford, with only three denials. In addition, of the fifteen insurers, only two companies approved the recommended treatment; these insurers were Genex and MyMatrixx. As shown in Table 1 below, the insurers with the greatest amounts of UR resubmissions included Sedgwick with 87 submissions, Arbicare with nineteen submissions, and My Matrixx with twelve submissions.
Requested treatment
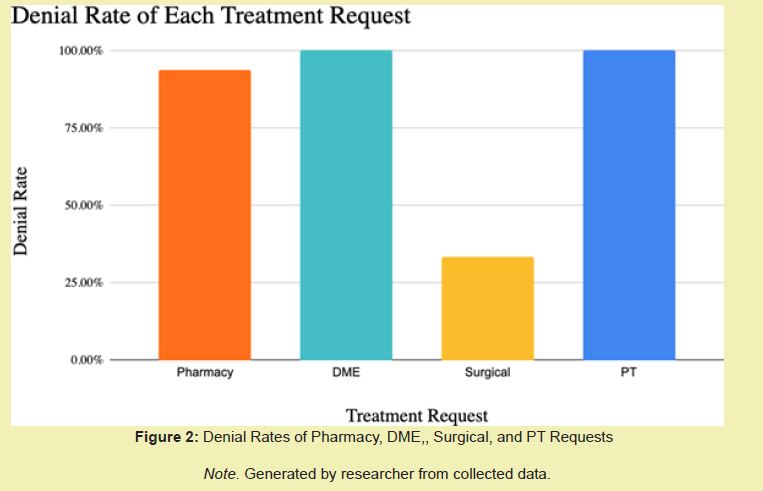
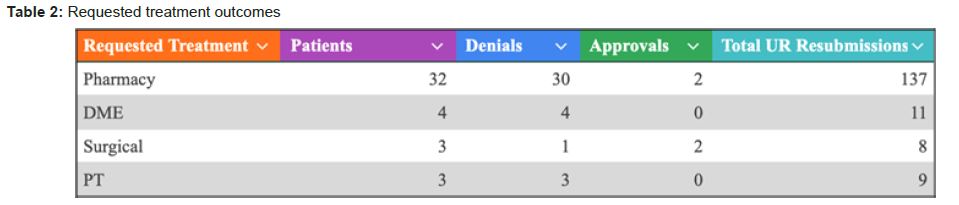
Regarding each type of requested treatment, the majority of WC patients received pharmacy-related requests. Notably, the average number of UR resubmissions pertaining to each treatment was 4.28 per patient for pharmacy, 2.75 per patient for DME, 2.67 per patient for surgical, and 3.00 per patient for PT.
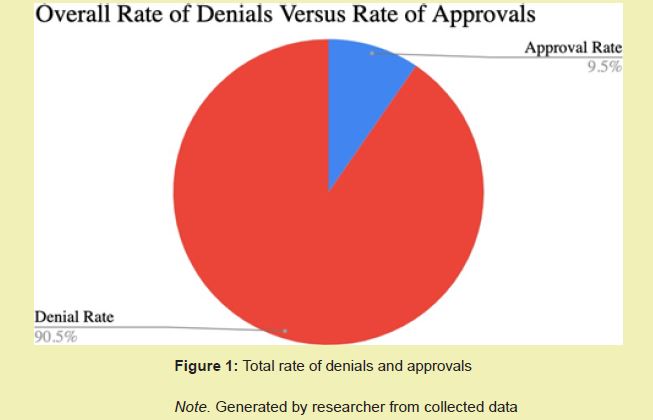
Despite following the requirements of the Illinois WC Act, only a 9.52% approval rate was achieved. Each of the approved treatments was reported as being paid by their given insurer. On the contrary, the denial rate reached a much greater percentage of 90.48%.
For each requested treatment, the majority of patients subjected to the UR process obtained pharmacy treatment-related requests. The rate of denial was reflected through each treatment, with pharmacy requests reaching a 93.75% denial rate. The number of patients with durable medical equipment, physical therapy, and surgical requests was much lower in comparison to the number of patients with pharmaceutical treatment requests. DME treatments had a 100% denial rate amongst the four patients with this requested treatment. Likewise, PT requests also had a 100% denial rate for the three patients obtaining this treatment request. Of the three patients with surgical treatment requests, only one of them was denied, providing this treatment request with only a 33.33% denial rate Figure1, Figure 2.
The average time between a UR denial and a subsequent response by the insurance company was 124 days. The standard deviation of the wait times was 52.12. On average, the patients that were approved had 2.75 UR submissions each, whereas the patients that faced repeat denials had 4.05 submissions each.
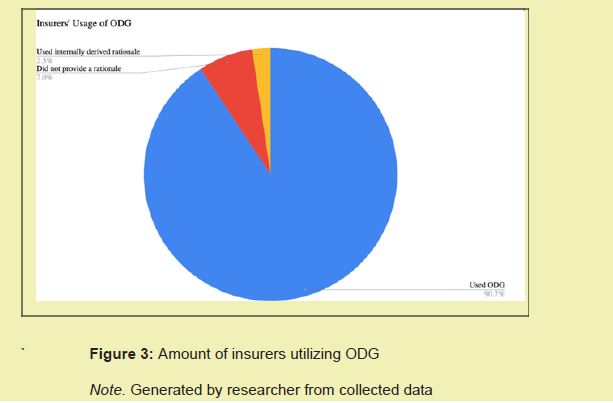
Clinical guidelines utilized
90.48% of the insurance companies reported using ODG to review the UR submissions, with one insurance company following only their internal review guidelines. Seven insurers did not cite their clinical guidelines which falls outside of the Illinois WC act. One company, Zurich, used internal clinical rationale, which falls outside of the requirements of the WC Act stating that they are meant to use nationally recognized clinical guidelines Figure 3.
Insurance provider denials
Workers’ compensation intends to provide timely and appropriate medical care to the injured worker injured at no fault of their own. Even though the requested medical treatment was reasonable and necessary, and all aspects of the Utilization Review process were followed by the treating physician, only an approval rate of 9.09% was achieved, in addition to an average of about four months spent in the UR process. These results demonstrate that when an insurance company enacts the UR process, access to care is significantly diminished. Ultimately, WC was set up as a no-fault system to provide timely access to medical treatment for the injured worker. However, as presented by the findings of this study, 90.48% of the reviewed WC patients were denied treatment and, therefore, were unable to access their necessary treatment. Furthermore, of the fifteen recorded insurance providers, Sedgwick had the largest number of patients and displayed the greatest number of denials and UR resubmissions. Only two insurers of the fifteen approved the requested treatment, providing four out of the 42 patients with care. These results point to the larger trend of an insurer’s likelihood to deny a requested treatment, despite the treatment being necessary and proper. Insurance companies' concerns include faulty claims increasing insurance costs which ultimately are passed onto the consumer, leading to this aforementioned trend of repeat denials. However, calling back to the information provided by the National Council on Compensation Insurance, the frequencies of WC claims over $1 million have been decreasing by 3% each year as of 2002, thereby proving that the cost of WC has decreased over time.13
Requested treatment
As displayed in Table 2, the majority of patients who were subjected to UR were seeking pharmacy approvals. Of the 42 patients subjected to UR, 32 of them were assigned pharmaceutical treatment requests. This outcome demonstrates that pharmaceutical treatment requests have a higher chance of being reviewed through the UR process, requiring more UR resubmissions from the treating physician. Pharmacy requests had an average of about 4.28 resubmissions, whereas surgical and DME requests had an average of only 2.75 resubmissions for each patient. From these data points, it can be inferred that WC patients in need of pharmaceutical treatment may face greater waiting times and denials; therefore, it is exemplified that the UR process poses greater hindrances to patients with pharmacy treatment requests.
Building on this idea, the patients that were approved had, on average, fewer UR resubmissions than the patients that were denied. This finding supports that an overwhelming majority of the reviewed patients—90.48%—experienced significant delays in their treatment due to repeat denials. On average, each denied patient experienced a waiting time of 124 days, furthering the aforementioned point that delays are evident within the UR process. The higher the denial rate and longer wait times are harmful to the patient since they are unable to receive the treatment they need for their given injury in a timely manner.
Clinical guidelines utilized
Of the fifteen reviewed insurance companies, one company did not comply with the Illinois WC Act, stating that nationally recognized guidelines must be utilized. This finding proposes an issue since the reviewed orthopedic practice complied with the WC Act throughout the UR submission process, but was met with the insurer’s noncompliance with the state requirements. Despite 90.48% of the insurers using the ODG, only a 9.52% approval rate was met. Based on this data, a concern surrounding the efficiency and applicability of the ODG is raised. Without beneficial nationally recognized guidelines, WC patients will continue to face delays and denials for their treatment, and from this, many patients will have no means of seeking necessary care or compensation for lost work days.
Implications
The results displaying the impacts of UR processes on WC denials highlights a clear trend that insurers implement UR as a method to limit access to appropriate medical treatment as a means to limit their costs and not necessarily improve treatment for the injured workers. Even though the insurance companies have been concerned about runaway WC costs, the aforementioned ProPublica study on decreasing WC benefits demonstrated that the average WC cost to employers for every $100 of workers’ wages has decreased by $1.23 from 1988 to 2014.12
The treating physician from this study’s reviewed orthopedic practice participated in the UR process and explained that the medical reasoning was appropriate and necessary; however, only 9.52% approval rate on recommended treatment was achieved with an average of 124 days involved in the UR process. These findings are consistent with those of the meta-analysis published in the Journal of Occupational Rehabilitation in 2024, which reported that 13.3% of workers in the United States have encountered difficulties accessing care.10
Connecting the findings of the case series back to the 2001 study published in Journal of Risk and Insurance, Jeff Biddle found that more aggressive denial policies, a factor displayed in this case series, lead to less individuals filing for WC.8 These shortcomings of the UR process contribute to the increasing denial rates and decreasing costs of WC, ultimately, necessitating revisions in the UR process that provide patients with the care they need.
Given the alignment of the reported data with findings from other studies of similar scope, it is evident that insurers need to implement changes into their UR processes that ensure injured workers have access to necessary care. Such changes could include a more timely response to the appeal process by the treating physician. As long as the treating physician appropriately submits to the UR process and aligns with the clinical rationale, it is in the insurer's best interest to have an appeal and approval process such that patients can receive their timely and appropriate medical treatment for their WC injury.21
Limitations include a limited scope on the UR process for a range of patients subjected to UR from January 1, 2024 to December 1, 2024. Given that documentations were provided by only one orthopedic practice, the researcher was limited to the 42 patients facing UR over the given time period. In addition, a possible correspondence to insurers’ likelihood of denying patients from a specific practice may be applicable in this scenario, but cannot be evaluated due to the fact that the patient histories are each from the same practice.22
To overcome this limitation, future researchers could select multiple orthopedic practices to review the cases of patients facing UR over a given period of time. This could shed light on whether or not insurance companies uphold biases pertaining to a specific practice. Utilizing more practices would also provide the researcher with more patient data to survey and more variables to track. To take this idea even further, future researchers could also review other types of practices that receive a large quantity of WC patients. With a wider range of injury types, the researcher could review more requested treatment types and how the trends of denials and approvals correspond with other practices’.
None.
This Research Article received no external funding.
Regarding the publication of this article, the author declares that he has no conflict of interest.
- 1. Tyrkus MJ, Schwartz. Workers' Compensation. In MJ Tyrkus & C. A. Schwartz (Eds.), Gale Encyclopedia of American Law. Gale. 2022;10:489-494.
- 2. Burriesci J. Historical Summary of Workers’ Compensation Laws. Connecticut General Assembly, Office of Legislative Research. 2001.
- 3. What Is Workers’ Compensation Process In California?” Santa Clara County Workplace Injury Claims Attorneys. 2024.
- 4. Parsons C. Liability Rules, Compensation Systems and Safety at Work in Europe. The Geneva Papers on Risk and Insurance. 2002;27(3):358-382.
- 5. Bean M, Erdil M, Blink R, et al. Utilization Review in Workers' Compensation: Review of Current Status and Recommendations for Future Improvement. Journal of occupational and environmental medicine. 2020;62(6):e273-e286.
- 6. State Adoptions. ODG by MCG. 2004.
- 7. Illinois General Assembly. Illinois Compiled Statutes. ILCS Database. 2023.
- 8. Biddle J. Do High Claim-Denial Rates Discourage Claiming? Evidence from Workers Compensation Insurance. The Journal of Risk and Insurance. 2001;68(4):631-658.
- 9. Gold AE, Gilbert A, McMichael BJ. Socially Distant Health Care. Tulane Law Review. 2002;96(3):423-468.
- 10. Mekonnen TH, Di Donato M, Collie A, et al. Time to Service and Its Relationship with Outcomes in Workers with Compensated Musculoskeletal Conditions: A Scoping Review. Journal of occupational rehabilitation. 2024;34(3):522-554.
- 11. Card D, McCall BP. Is Workers’ Compensation Covering Uninsured Medical Costs? Evidence from the “Monday Effect.” ILR Review. 1996;49(4):690-706.
- 12. Grabell M. The Demolition of Workers’ Comp. ProPublica. 2015.
- 13. Bernard N. Understanding Loss Cost Actions. NCCI. 2024.
- 14. State and federal worker compensation benefits U.S. 2020.” Statista. 2020.
- 15. Glass LS, Blink RC, Bean M, et al. Utilization Review in Worker’s Compensation: Current Status and Opportunities for Improvement. Journal of occupational and environmental medicine. 2017;59(10):1024-1026.
- 16. Rauner B, Fratianni J. State of Illinois Workers’ Compensation Commission Fiscal Year 2017 Annual Report.” 2024.
- 17. Daniels AH, Kuris EO, Palumbo MA. The Role of the Orthopaedic Surgeon in Workers' Compensation Cases. The Journal of the American Academy of Orthopaedic Surgeons. 2017;25(3):e45-e52.
- 18. Eric C Makhni, Richard Li, Charles S Day. American Journal of Orthopedics. 2011.
- 19. Remppis J, Ganzenmueller T, Kohns Vasconcelos M, et al. A case series of children and young people admitted to a tertiary care hospital in Germany with COVID-19. BMC Infect Dis. 2021;21:133.
- 20. Hamm RM, Reiss DM, Paul RK, et al. Knocking at the wrong door: Insured workers’ inadequate psychiatric care and workers’ compensation claims. International Journal of Law and Psychiatry. 2007;30(4-5):416-426.
- 21. NCI Dictionary of Cancer Terms. 2024.
- 22. The Share of Americans Without Health Insurance in 2023 Remained Low. Peterson Foundation. 2024.

